Hypertension
Introduction and Facts
Hypertension increases systolic blood pressure greater than 140 mmHg and/or diastolic more significant than 90 mmHg on two measurements with an interval of 5 minutes in a state of sufficient rest (calm). Hypertension is defined by the Joint National Committee on Detection, Evaluation, and Treatment of High Blood Pressure as pressure higher than 140/90 mmHg. Based on the cause of hypertension is divided into two groups, namely:
1) Essential hypertension, or primary hypertension with no known cause, is also called idiopathic hypertension. There are about 95% of cases.
2) Secondary hypertension or renal hypertension. There are about 5% of cases. The specific causes are known, such as estrogen use, renal disease, renal vascular hypertension, primary hyperaldosteronism and Cushing's syndrome, pheochromocytoma, coarctation of the aorta, pregnancy-related hypertension, and others.
Pathophysiology
The body has a system that functions to prevent acute changes in blood pressure caused by circulatory disorders, which tries to maintain blood pressure stability in the long-term cardiovascular reflexes through the nervous system, including the control system that reacts immediately. Long-term blood pressure stability is maintained by a system that regulates body fluids that involve various organs, especially the kidneys.
1) Changes in the anatomy and physiology of blood vessels (atherosclerosis) are disorders characterized by thickening and loss of elasticity of the arteries. Atherosclerosis is a multifactorial process. Inflammation occurs in the walls of blood vessels, and deposits of fatty substances, cholesterol, cellular waste products, calcium, and various other substances are formed in the lining of the blood vessels. These growths are called plaques. The development of plaque under the tunica intima layer will reduce the lumen of blood vessels, luminal obstruction, blood flow abnormalities, reduced oxygen supply to specific organs or body parts. Vascular endothelial cells also have an essential role in controlling cardiac blood vessels by producing local vasoactive nitric oxide molecules and endothelium peptides. Endothelial dysfunction is joint in cases of primary hypertension.
2) The renin-angiotensin system. The mechanism of hypertension is through the formation of angiotensin II from angiotensin I by angiotensin I-converting enzyme (ACE). Angiotensin II has a crucial role in raising blood pressure through two main actions: Increased secretion of Anti-Diuretic Hormone (ADH) and thirst. And the second is to stimulate aldosterone secretion from the adrenal cortex.
3) Sympathetic nervous system. The mechanisms that control the constriction and relaxation of blood vessels are located in the vasomotor center, in the medulla in the brain. There will be a release of acetylcholine with sympathetic nerve stimulation, which will stimulate post-ganglionic nerve fibers to the blood vessels, where the release of norepinephrine causes blood vessel constriction.
Clinical Symptoms and Complications
On physical examination, there were no abnormalities other than high blood pressure. Still, changes in the retina can also be found, such as bleeding, exudate, narrowing of blood vessels, and in severe cases, pupillary edema (optic disc edema) can be found.
According to Price, the symptoms of hypertension include headaches, neck stiffness, difficulty sleeping, restlessness, headaches, chest palpitations, weakness, shortness of breath, sweating, and dizziness (Price, 2005).
Symptoms of the disease usually occur both in people with hypertension and in someone with normal blood pressure hypertension are headaches, restlessness, palpitations, nosebleeds, difficulty sleeping, shortness of breath, irritability, ringing in the ears, and heavy bending pounding and frequent urination at night. Symptoms due to complications of hypertension that have ever been encountered include impaired vision, nerves, heart, kidney function, and cerebral (brain) disorders that result in seizures and bleeding of cerebral blood vessels that result in paralysis and impaired consciousness to coma (Cahyono, 2008).
Corwin states that most of the clinical symptoms that arise after experiencing hypertension for years are headaches when awake, sometimes accompanied by nausea and vomiting caused by increased intracranial blood pressure (Corwin, 2005).
Diagnosis
The most accurate physical examination is using a sphygmomanometer. It is advisable to take more than one measurement in a sitting position with the elbows bent on the table with the palms facing up, and the arms should be at heart level. Other investigations may also be required if necessary.
Medication and Treatment
There are five groups of first-line drugs commonly used for the initial treatment of hypertension, namely diuretics, beta-adrenergic receptor blockers (β-blockers), angiotensin-converting enzyme (ACE-inhibitors) inhibitors, and angiotensin receptor blockers (Angiotensin Receptor Blockers). /ARB) and calcium antagonists. In addition, three groups of drugs are considered second-line, namely: adrenergic nerve blockers, central -2 agonists, and vasodilators (Nafrialdi, 2009).
1. Diuretics work to increase sodium, water, and chloride excretion, thereby reducing blood volume and extracellular fluid. As a result, there is a decrease in cardiac output and blood pressure.
2. Adrenergic Blockers
a. Beta Adrenoreceptor Blockers (β-Blockers)
b. Alpha Adrenoceptor Blockers (α-Blockers)
3. Vasodilators, several drugs belong to the vasodilator group, including hydralazine, minoxidil, diazoxide, and sodium nitroprusside. Side effects that often occur in the administration of this drug are dizziness and headaches (Depkes, 2006).
4. Angiotensin-Converting Enzyme Inhibitors (ACE-Inhibitors), for example, benazepril, captopril, enalapril, fosinopril, lisinopril, moexipril, perindopril, quinapril, ramipril, trandolapril, and tanapres (Benowitz, 2002).
5. Angiotensin II Receptor Antagonists (Angiotensin Receptor Blockers, ARBs), including kandersartan, eprosartan, irbesartan, losartan, olmesartan, telmisartan and valsartan (MOH, 2006)
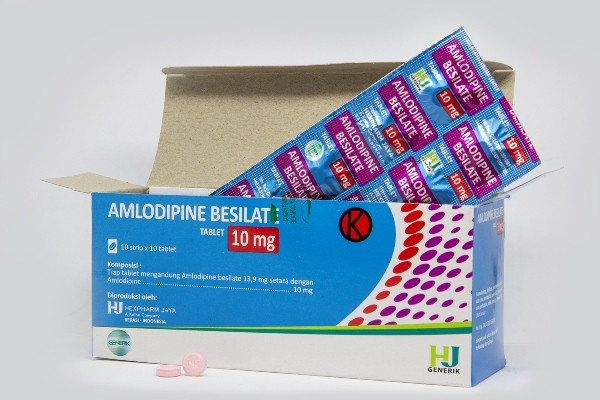
6. Calcium channel blocker (CCB) antagonists dihydropyridine (nifedipine, amlodipine, verapamil, and benzothiazepine).
7. Sympathetic blockers, for example, methyldopa, clonidine, and reserpine.
Control of risk factors for coronary heart disease that can influence the occurrence of hypertension is only limited to risk factors that can be changed, with the following efforts:
a. Overcoming obesity / losing excess weight
b. Reduce salt intake in the body
c. Create a relaxed state
d. Doing regular exercise
e. Quit smoking
f. Reduce / stop alcohol consumption
Reference:
Hypertension [Internet]. Available from: http://eprints.undip.ac.id/43896/3/Gilang_YA_G2A009181_Bab2KTI.pdf
Hypertension.[Internet]. Available from: http://digilib.unila.ac.id/2440/9/BAB%20II.pdf