Sindrom Koroner Akut
Pendahuluan dan Fakta
Sindrom Koroner Akut (SKA) merupakan suatu masalah kardiovaskular yang utama karena menyebabkan angka perawatan rumah sakit dan angka kematian yang tinggi. Banyak kemajuan yang telah dicapai melalui penelitian dan oleh karenanya diperlukan pedoman tatalaksana sebagai rangkuman penelitian yang ada.
Patofisiologi
Sebagian besar SKA adalah manifestasi akut dari plak ateroma pembuluh darah koroner yang koyak atau pecah. Hal ini berkaitan dengan perubahan komposisi plak dan penipisan tudung fibrus yang menutupi plak tersebut. Kejadian ini akan diikuti oleh proses agregasi trombosit dan aktivasi jalur koagulasi. Terbentuklah trombus yang kaya trombosit (white thrombus). Trombus ini akan menyumbat liang pembuluh darah koroner, baik secara total maupun parsial; atau menjadi mikroemboli yang menyumbat pembuluh koroner yang lebih distal. Selain itu terjadi pelepasan zat vasoaktif yang menyebabkan vasokonstriksi sehingga memperberat gangguan aliran darah koroner. Berkurangnya aliran darah koroner menyebabkan iskemia miokardium. Pasokan oksigen yang berhenti selama kurang-lebih 20 menit menyebabkan miokardium mengalami nekrosis (infark miokard).
Infark miokard tidak selalu disebabkan oleh oklusi total pembuluh darah koroner. Obstruksi subtotal yang disertai vasokonstriksi yang dinamis dapat menyebabkan terjadinya iskemia dan nekrosis jaringan otot jantung (miokard). Akibat dari iskemia, selain nekrosis, adalah gangguan kontraktilitas miokardium karena proses hibernating dan stunning (setelah iskemia hilang), distritmia dan remodeling ventrikel (perubahan bentuk, ukuran dan fungsi ventrikel). Sebagian pasien SKA tidak mengalami koyak plak seperti diterangkan di atas. Mereka mengalami SKA karena obstruksi dinamis akibat spasme lokal dari arteri koronaria epikardial (Angina Prinzmetal). Penyempitan arteri koronaria, tanpa spasme maupun trombus, dapat diakibatkan oleh progresi plak atau restenosis setelah Intervensi Koroner Perkutan (IKP). Beberapa faktor ekstrinsik, seperti demam, anemia, tirotoksikosis, hipotensi, takikardia, dapat menjadi pencetus terjadinya SKA pada pasien yang telah mempunyai plak aterosklerosis.
Gejala Klinis dan Komplikasi
Keluhan pasien dengan iskemia miokard dapat berupa nyeri dada yang tipikal (angina tipikal) atau atipikal (angina ekuivalen).
Keluhan angina tipikal berupa rasa tertekan/berat daerah retrosternal, menjalar ke lengan kiri, leher, rahang, area interskapular, bahu, atau epigastrium. Keluhan ini dapat berlangsung intermiten/beberapa menit atau persisten (>20 menit). Keluhan angina tipikal sering disertai keluhan penyerta seperti diaphoresis, mual/muntah, nyeri abdominal, sesak napas, dan sinkop
Presentasi angina atipikal yang sering dijumpai antara lain nyeri di daerah penjalaran angina tipikal, rasa gangguan pencernaan (indigestion), sesak napas yang tidak dapat diterangkan, atau rasa lemah mendadak yang sulit diuraikan. Keluhan atipikal ini lebih sering dijumpai pada pasien usia muda (25-40 tahun) atau usia lanjut (>75 tahun), wanita, penderita diabetes, gagal ginjal menahun, atau demensia.
Diagnosis SKA menjadi lebih kuat jika keluhan tersebut ditemukan pada pasien dengan karakteristik sebagai berikut :
1. Pria
2. Diketahui mempunyai penyakit aterosklerosis non koroner (penyakit arteri perifer / karotis)
3. Diketahui mempunyai PJK atas dasar pernah mengalami infark miokard, bedah pintas koroner, atau IKP
4. Mempunyai faktor risiko: umur, hipertensi, merokok, dislipidemia, diabetes mellitus, riwayat PJK dini dalam keluarga, yang diklasifikasi atas risiko tinggi, risiko sedang, risiko rendah menurut NCEP (National Cholesterol Education Program)
Diagnosis
Dengan mengintegrasikan informasi yang diperoleh dari anamnesis, pemeriksaan fisik, elektrokardiogram, tes marka jantung, dan foto polos dada, diagnosis awal pasien dengan keluhan nyeri dada dapat dikelompokkan sebagai berikut: non kardiak, Angina Stabil, Kemungkinan SKA, dan Definitif SKA
Pemeriksaan fisik. Pemeriksaan fisik dilakukan untuk mengidentifikasi faktor pencetus iskemia, komplikasi iskemia, penyakit penyerta dan menyingkirkan diagnosis banding. Regurgitasi katup mitral akut, suara jantung tiga (S3), ronkhi basah halus dan hipotensi hendaknya selalu diperiksa untuk mengidentifikasi komplikasi iskemia. Ditemukannya tanda-tanda regurgitasi katup mitral akut, hipotensi, diaphoresis, ronkhi basah halus atau edema paru meningkatkan kecurigaan terhadap SKA.
Pemeriksaan elektrokardiogram. Semua pasien dengan keluhan nyeri dada atau keluhan lain yang mengarah kepada iskemia harus menjalani pemeriksaan EKG 12 sadapan sesegera mungkin sesampainya di ruang gawat darurat. Sebagai tambahan, sadapan V3R dan V4R, serta V7-V9 sebaiknya direkam pada semua pasien dengan perubahan EKG yang mengarah kepada iskemia dinding inferior. Sementara itu, sadapan V7-V9 juga harus direkam pada semua pasien angina yang mempunyai EKG awal nondiagnostik. Sedapat mungkin, rekaman EKG dibuat dalam 10 menit sejak kedatangan pasien di ruang gawat darurat. Pemeriksaan EKG sebaiknya diulang setiap keluhan angina timbul kembali.
Pemeriksaan marka jantung. Kreatinin kinase-MB (CK-MB) atau troponin I/T merupakan marka nekrosis miosit jantung dan menjadi marka untuk diagnosis infark miokard. Troponin I/T sebagai marka nekrosis jantung mempunyai sensitivitas dan spesifisitas lebih tinggi dari CK-MB. Peningkatan marka jantung hanya menunjukkan adanya nekrosis miosit, namun tidak dapat dipakai untuk menentukan penyebab nekrosis miosit tersebut (penyebab koroner/nonkoroner). Troponin I/T juga dapat meningkat oleh sebab kelainan kardiak nonkoroner seperti takiaritmia, trauma kardiak, gagal jantung, hipertrofi ventrikel kiri, miokarditis/perikarditis.
Pemeriksaan laboratorium. Data laboratorium, di samping marka jantung, yang harus dikumpulkan di ruang gawat darurat adalah tes darah rutin, gula darah sewaktu, status elektrolit, koagulasi darah, tes fungsi ginjal, dan panel lipid. Pemeriksaan laboratorium tidak boleh menunda terapi SKA.
Pemeriksaan foto polos dada. Mengingat bahwa pasien tidak diperkenankan meninggalkan ruang gawat darurat untuk tujuan pemeriksaan, maka foto polos dada harus dilakukan di ruang gawat darurat dengan alat portabel. Tujuan pemeriksaan adalah untuk membuat diagnosis banding, identifikasi komplikasi dan penyakit penyerta.
Berdasarkan anamnesis, pemeriksaan fisik, pemeriksaan elektrokardiogram (EKG), dan pemeriksaan marka jantung, Sindrom Koroner Akut dibagi menjadi:
1. Infark miokard dengan elevasi segmen ST (STEMI: ST segment elevation myocardial infarction)
2. Infark miokard dengan non elevasi segmen ST (NSTEMI: non ST segment elevation myocardial infarction)
3. Angina Pektoris tidak stabil (UAP: unstable angina pectoris)
Tatalaksana dan Perawatan
Tata Laksana
Tata laksana pada sindrom koroner akut mencakup beberapa strategi, berdasarkan tingkat keparahan dan jenis SKA, seperti ST elevasi pada miokard infark (STEMI) atau non ST elevasi pada miokard infark (NSTEMI). Beberapa langkah di antaranya adalah:
- Terapi Oksigen: Untuk pasien dengan hipoksemia (saturasi oksigen <90%). Terapi oksigen rutin tidak disarankan untuk pasien dengan kadar oksigen normal.
- Nitrat: Nitrat sublingual dapat diberikan untuk meredakan nyeri dada iskemik. Namun, penggunaannya harus hati-hati, terutama pada pasien dengan hipotensi atau menggunakan inhibitor phosphodiesterase.
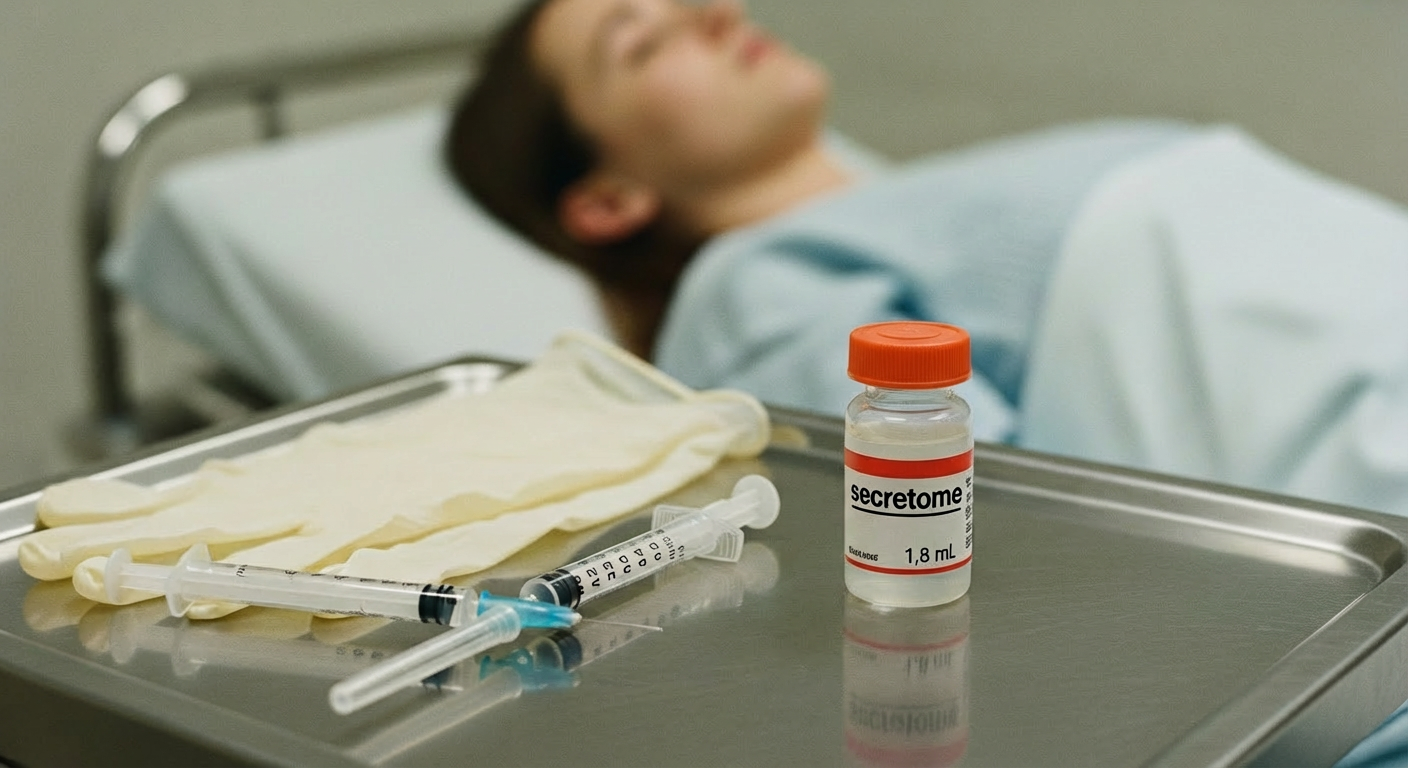
- Pemberian opioid intravena seperti morfin digunakan untuk meredakan nyeri dada yang parah, meskipun bisa memperlambat penyerapan obat oral.
- Pemberian beta-blocker intravena, seperti metoprolol, direkomendasikan untuk pasien yang menjalani intervensi percutaneous coronary intervention (PCI) primer jika tidak ada tanda-tanda gagal jantung akut dan tekanan darah sistolik di atas 120 mmHg.
- Terapi Antitrombotik:
- Antiplatelet: Penggunaan aspirin dimulai dengan dosis awal (loading dose), diikuti dengan dosis pemeliharaan. Inhibitor P2Y12 seperti clopidogrel, prasugrel, atau ticagrelor direkomendasikan, terutama untuk pasien yang menjalani PCI.
- Antikoagulan: Heparin tak terfraksionasi atau unfractionated heparin (UFH), enoxaparin, atau fondaparinux dapat digunakan sebagai antikoagulan dalam fase akut SKA.
- Terapi Reperfusi (PCI atau Fibrinolisis): Percutaneous coronary intervention (PCI) primer adalah strategi reperfusi yang disarankan untuk pasien STEMI, yang dapat dilakukan dalam waktu 120 menit setelah diagnosis. Jika tidak memungkinkan, maka fibrinolisis direkomendasikan.
- Terapi Fibrinolitik: Fibrinolisis harus dimulai pada pasien STEMI yang tidak dapat menjalani PCI dalam waktu yang disarankan. Agen seperti tenekteplase atau alteplase digunakan.
Referensi:
- Perhimpunan Dokter Spesialis Kardiovaskuler Indonesia. Pedoman tatalaksana sindrom koroner akut. [Internet]. [Cited 27/8/2021]. Available from: https://inaheart.org/wp-content/uploads/2021/07/Pedoman_tatalaksana_Sindrom_Koroner_Akut_2015.pdf
- European Society of Cardiology (ESC). 2023 ESC Guidelines for the management of acute coronary syndromes. European Heart Journal. 2023;00:1-107. DOI: https://doi.org/10.1093/eurheartj/ehad191