Osteoporosis
Introduction and Facts
Osteoporosis is a major global health problem causing more than 200 million osteoporotic fractures worldwide each year, including 1.6 million hip fractures. In the United States in 2005, there were an estimated two million osteoporosis-related fractures, including approximately 547,000 spine fractures, 297,000 hip fractures, 397,000 wrist fractures, 135,000 pelvic fractures, and 675,000 hip fractures. At another place. The total number of fractures in the United States will reach more than 3 million by 2025.
According to the 1993 International Consensus Definition, osteoporosis is a systemic skeletal disease characterized by low bone mass and microarchitectural damage to bone tissue, resulting in bone fragility and increased fracture susceptibility. In 2001, the National Institute of Health (NIH) proposed a new definition of osteoporosis as a systemic bone disease characterized by compromised bone strength so that bones break easily. Osteoporosis is operationally defined based on the assessment of bone mineral density (BMD). Based on WHO criteria, osteoporosis is a BMD value that is at 2.5 standard deviations (SD) or below the average value for healthy young adults (T score < -2.5 SD).
Pathophysiology/ Pathogenesis
Osteoporosis occurs due to a disturbance in the balance between bone resorption and bone formation processes, which is cellularly caused by the number and activity of osteoclasts (bone resorption cells) exceeding the number and activity of osteoblasts (bone formation cells). This condition results in a decrease in bone mass. Osteoporosis is divided into two groups, namely primary (involutional) osteoporosis, and secondary osteoporosis. Primary osteoporosis is osteoporosis with no known cause. Secondary osteoporosis is osteoporosis with a known cause. Primary osteoporosis is divided into 2, namely osteoporosis type I (formerly known as post-menopausal osteoporosis) and osteoporosis type II (formerly known as senile osteoporosis). In the 1990s, Riggs and Melton suggested that estrogen is essential in the onset of primary osteoporosis in post-menopausal and senile.
Estrogen is an essential regulator of bone growth and homeostasis. Estrogen plays a significant role in bone metabolism, influencing the activity of osteoblasts or osteoclasts, including maintaining the balance of work of these two cells. The indirect effect of estrogen on bone is related to calcium homeostasis, including calcium absorption in the intestine, modulation of 1,25(OH)2 vitamin D, renal calcium excretion, and parathyroid hormone secretion.
Clinical Symptoms and Complications
Clinical symptoms can be found by history and physical examination. The introduction of risk factors for osteoporosis will be beneficial in approaching the diagnosis of osteoporosis. The risk factors for osteoporosis are age, genetics, environment, endogenous hormones, chronic diseases, and the physical characteristics of the bones.
Diagnosis
Until now, early detection of osteoporosis is a challenging thing to do. Osteoporosis is a silent disease; sometimes, there are no signs or symptoms before a fracture occurs.
For the diagnosis of osteoporosis, include:
a. History: a doctor should be aware of the possibility of osteoporosis if there are: 1) fractures due to minor trauma, 2) body shortening, dorsal kyphosis increases, bone pain, 3) incidentally found characteristic radiological features. Clinical evaluation of patients with osteoporosis is directed at identifying risk factors.
b. Supporting investigation
1) Laboratory examination in the form of biochemical bone markers
Radiological determination of bone mass is essential in determining the diagnosis of osteoporosis. Still, it does not provide an overview of the dynamic processes of bone resorption and formation, which can indicate the degree of the speed of bone loss. Bone biopsy and biochemical parameters can provide this picture, but bone biopsy is an invasive procedure, making it difficult to perform routinely for screening and monitoring treatment. Thus, the only option for determining bone turnover is biochemical parameters or markers.
Bone biochemical markers for bone turnover (biochemical bone markers) are distinguished for the operation of bone formation and resorption. The Expert Committee of the Committee of Scientific Advisors of the International Osteoporosis Foundation, recommends in post-menopausal osteoporosis with hormone replacement therapy or bisphosphonates, by measuring 1 or 2 parameters, respectively the process of bone formation and resorption, namely osteocalcin, BSAP, P1NP for bone formation, as well as -Cross Laps (CTx) and U-DPD for bone resorption.
2) Radiological examination
Radiological examination to assess bone density is not very sensitive.
The diagnostic value of the regular radiological examination to assess early osteoporosis is not satisfactory. This examination can only detect osteoporosis after a decrease in more than 30% bone mass density. The characteristic radiological features of osteoporosis are cortical thinning and a more lucent trabecular area. This will be seen in the vertebral bones, which provide a picture-frame picture of the vertebrae. In the vertebral column, anteroposterior and lateral radiographs are excellent for looking for compression fractures, wedge fractures, or biconcave fractures.
3) Check the bone mass density
Bone densitometry is an accurate and precise examination to assess bone mass density, so it can be used to evaluate prognostic factors, fracture prediction, and diagnosis of osteoporosis. Various methods that can be used to assess bone mass are single-photon absorptiometry (SPA), dual photon absorptiometry (DPA), X-ray Absorptiometry (there are two types, namely Single X-ray Absorptiometry = SXA and Dual Energy X-ray Absorptiometry = DEXA). ) and quantitative computer tomography (QCT).
Management and Treatment
Osteoporosis management includes preventive measures and early treatment, thereby preventing complications of bone fragility fractures.
Non-Pharmacology
1. Education and Prevention
Osteoporosis can affect anyone, including individuals who are very careful about their lifestyle, eat right, exercise regularly, don't smoke, don't drink alcohol or only drink small amounts, and don't have any diseases, conditions, use of alcohol, or drugs that may predispose to osteoporosis. Osteoporosis patients whose lifestyles are erratic should be counseled about all their activities of daily living to allow for slowing the progression of bone loss.
2 Exercise and rehabilitation program
Exercise and rehabilitation programs are essential for people with osteoporosis. With regular exercise, patients will be more agile, agile, and strong in their muscles, so they are not easy to fall. In addition, exercise will also prevent the worsening of osteoporosis because there are biophysicoelectrochemical stimuli that will increase bone remodeling.
Pharmacology
Theoretically, osteoporosis can be treated by inhibiting the action of osteoclasts and or increasing the work of osteoblasts. However, currently circulating drugs are generally anti-resorption, including anti-resorption drugs such as estrogen, calcitonin, and bisphosphonates. At the same time, Calcium and Vitamin D do not have anti-resorption or bone stimulator effects but are needed to optimize osteoid neutralization after bone formation by osteoblast cells.
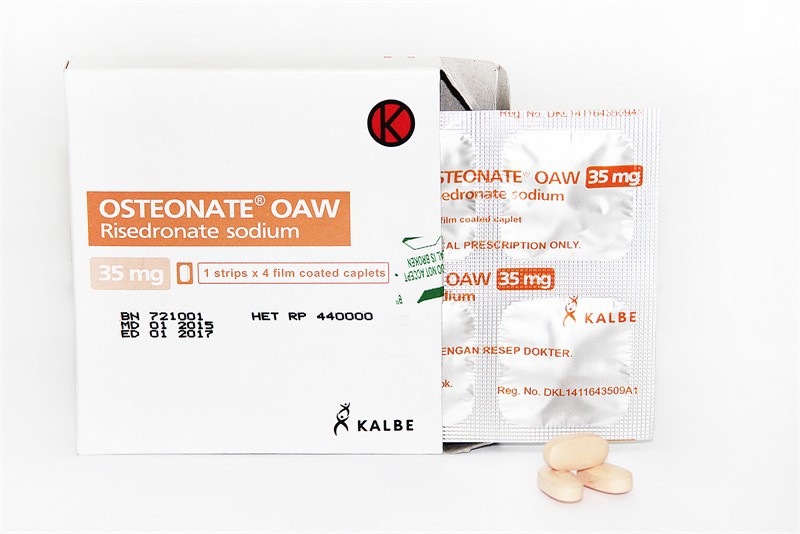
1. Bisphosphonates
Bisphosphonates are drugs used to treat osteoporosis. Bisphosphonates are pyrophosphate analogs consisting of 2 phosphonic acids bonded to each other by carbon atoms. Bisphosphonates can reduce bone resorption by osteoclast cells by binding to the bone surface and inhibiting the action of osteoclasts by reducing the production of protons and lysosomal enzymes under osteoclasts.
2 Raloxifene
Raloxifene is an anti-estrogen preparation that has an estrogen-like effect on bone and lipids but does not cause stimulation of the endometrium and breast. Raloxifene is also known as a selective estrogen receptor modulator (SERM). This group acts on the beta-estrogen receptor, so it does not cause bleeding and the incidence of breast malignancy. The mechanism of action of Raloxifene on bone is thought to involve TGF-beta3 produced by osteoblasts which functions to inhibit osteoclast cell differentiation.
3. Estrogen
The mechanism of estrogen as an anti-resorption, affecting osteoblast cells or osteoclast cells, has been discussed previously. Administration of estrogen therapy in the prevention and treatment of osteoporosis is known as hormone replacement therapy (TSH). Estrogen is very well absorbed through the skin, vaginal mucosa, and gastrointestinal tract.
4. Calcitonin
Calcitonin is a drug that has been recommended by the FDA (Food and Drug Administration) for the treatment of diseases that increase bone resorption. The recommended dose for intranasal administration is 200 IU per day.
5. Strontium ranelate
Strontium ranelate is a dual-acting osteoporosis drug, which increases the work of osteoblasts and inhibits the creation of osteoclasts. The dose of strontium ranelate is 2 mg/day dissolved in water and given at night before bedtime or 2 hours before meals, or 2 hours after meals.
6. Vitamin D
Vitamin D plays a role in increasing the absorption of calcium in the intestine. More than 90% of vitamin D is synthesized in the body; its precursors are found under the skin by exposure to ultraviolet light. Vitamin D can be in the form of alfacalcidol (25 OH vitamin D3) and calcitriol (1,25 (OH)2 Vitamin D3), both of which can be used for the treatment of osteoporosis.
7. Calcitriol
Currently, calcitriol is not indicated as the first choice of treatment for postmenopausal osteoporosis. Calcitriol is indicated if there is hypocalcemia that does not improve with oral calcium administration. Calcitriol is also indicated to prevent secondary hyperparathyroidism, either due to hypocalcemia or terminal renal failure. The dose of calcitriol for the treatment of osteoporosis is 0.25 g, 1-2 times per day.
8. Calcium
Calcium as monotherapy was not sufficient to prevent fractures in patients with osteoporosis. The best calcium preparations are calcium carbonate because they contain elemental calcium 400 mg/gram, followed by calcium phosphate-containing elemental calcium 230 mg/gram, calcium citrate containing elemental calcium 211 mg/gram, calcium lactate containing elemental calcium 130 mg/gram, and calcium gluconate containing 90 mg/gram elemental calcium.
9. Phytoestrogens
Phytoestrogens are phytochemicals that have estrogenic activity. There are many phytoestrogen compounds, but what has been studied are isoflavones and lignans. Isoflavones that have an estrogenic effect include genistein, daidzein, and glycosides commonly found in legumes (Leguminosae) such as soybeans and red clover.
10. Parathyroid hormone
Intermittent administration of parathyroid hormone (PTH) can cause an increase in the number and activity of osteoblasts, resulting in an increase in bone mass and an improvement in bone microarchitecture. Teriparatide has been shown to reduce the risk of vertebral and non-vertebral fractures. The recommended dose is 20 g/day subcutaneously for 18-24 months.
11. Monoclonal antibody RANK-Ligand
As is known, osteoporosis is the result of the number and activity of osteoclast cells absorbing bone. In this case, biomolecular RANK-L plays a significant role. RANK-L will react with the RANK receptor on osteoclasts and form a RANK-RANKL complex, further increasing the differentiation and activity of osteoclasts. To prevent this reaction, monoclonal antibodies (MAbs) from RANK-L are used, known as denosumab.
Surgery
Surgery in patients with osteoporosis is performed if there is a fracture, especially a hip fracture.
Reference:
- Kristiningrum E. Farmakoterapi untuk osteoporosis. CDK 2020;47:41-8.
- Mukti M. Patogenesis, diagnosis dan penatalaksanaan osteoporosis [Internet]. 2011 [cited 2021 Aug 31]. Available from: http://docshare01.docshare.tips/files/14288/142889068.pdf