Rheumatoid Arthritis
Pendahuluan dan Fakta
Artritis Reumatoid atau Rheumatoid arthritis (RA) adalah penyakit autoimun sistemik (Symmons, 2006). RA merupakan salah satu kelainan multisistem yang etiologinya belum diketahui secara pasti dan dikarateristikkan dengan destruksi sinovitis (Helmick, 2008). Penyakit ini merupakan peradangan sistemik yang paling umum ditandai dengan keterlibatan sendi yang simetris (Dipiro, 2008). Penyakit RA ini merupakan kelainan autoimun yang menyebabkan inflamasi sendi yang berlangsung kronik dan mengenai lebih dari lima sendi (poliartritis) (Pradana, 2012).
Patofisiologi
RA merupakan penyakit autoimun sistemik yang menyerang sendi. Reaksi autoimun terjadi dalam jaringan sinovial. Kerusakan sendi mulai terjadi dari proliferasi makrofag dan fibroblas sinovial. Limfosit menginfiltrasi daerah perivaskular dan terjadi proliferasi sel-sel endotel kemudian terjadi neovaskularisasi. Pembuluh darah pada sendi yang terlibat mengalami oklusi oleh bekuan kecil atau sel-sel inflamasi. Terbentuknya pannus akibat terjadinya pertumbuhan yang iregular pada jaringan sinovial yang mengalami inflamasi. Pannus kemudian menginvasi dan merusak rawan sendi dan tulang Respons imunologi melibatkan peran sitokin, interleukin, proteinase dan faktor pertumbuhan. Respons ini mengakibatkan destruksi sendi dan komplikasi sistemik (Surjana, 2009). Sel T dan sel B merupakan respon imunologi spesifik. Sel T merupakan bagian dari sistem immunologi spesifik selular berupa Th1, Th2, Th17, Treg, Tdth, CTL/Tc, NKT. Sitokin dan sel B merupakan respon imunologi spesifik humoral, sel B berupa IgG, IgA, IgM, IgE, IgD (Baratwidjaja, 2012). Peran sel T pada RA diawali oleh interaksi antara reseptor sel T dengan share epitop dari major histocompability complex class II (MHCII-SE) dan peptida pada antigen-presenting cell (APC) pada sinovium atau sistemik. Dan peran sel B dalam imunopatologis RA belum diketahi secara pasti (Suarjana, 2009).
Gejala Klinis dan Komplikasi
Artritis Reumatoid (RA) dapat ditemukan pada semua sendi dan sarung tendo, tetapi paling sering di tangan. RA juga dapat menyerang sendi siku, kaki, pergelangan kaki dan lutut. Sinovial sendi, sarung tendo, dan bursa menebal akibat radang yang diikuti oleh erosi tulang dan destruksi tulang disekitar sendi (Syamsuhidajat, 2010). Ditinjau dari stadium penyakitnya, ada tiga stadium pada RA yaitu (Nasution, 2011):
a. Stadium sinovitis. Artritis yang terjadi pada RA disebabkan oleh sinovitis, yaitu inflamasi pada membran sinovial yang membungkus sendi. Sendi yang terlibat umumnya simetris, meski pada awal bisa jadi tidak simetris. Sinovitis ini menyebabkan erosi permukaan sendi sehingga terjadi deformitas dan kehilangan fungsi (Nasution, 2011). Sendi pergelangan tangan hampir selalu terlibat, termasuk sendi interfalang proksimal dan metakarpofalangeal (Suarjana, 2009).
b. Stadium destruksi. Ditandai adanya kontraksi tendon saat terjadi kerusakan pada jaringan sinovial (Nasution, 2011).
c. Stadium deformitas. Pada stadium ini terjadi perubahan secara progresif dan berulang kali, deformitas dan gangguan fungsi yang terjadi secara menetap (Nasution, 2011). Manifestasi klinis RA terbagi menjadi 2 kategori, yaitu manifestasi artikular dan manifestasi ekstraartikular (Suarjana, 2009). Manfestasi artikular RA terjadi secara simetris berupa inflamasi sendi, bursa, dan sarung tendo yang dapat menyebabkan nyeri, bengkak, dan kekakuan sendi, serta hidrops ringan (Sjamsuhidajat, 2010). Tanda kardinal inflamasi berupa nyeri, bengkak, kemerahan dan teraba hangat mungkin ditemukan pada awal atau selama kekambuhan, namun kemerahan dan perabaan hangat mungkin tidak dijumpai pada RA kronik (Surjana, 2009). Sendi-sendi besar, seperti bahu dan lutut, sering menjadi manifestasi klinis tetap, meskipun sendi-sendi ini mungkin berupa gejala asimptomatik setelah bertahun-tahun dari onset terjadinya (Longo, 2012)
Diagnosis
Untuk menegakkan diagnosis RA ada beberapa kriteria yang digunakan, yaitu kriteria diagnosis RA menurut American College of Rheumatology (ACR) tahun 1987 dan kriteria American College of Rheumatology/European League Against Rheumatism (ACR/EULAR)tahun 2010 (Pradana, 2012). Pemeriksaan laboratorium yang diperlukan untuk diagnosa RA antara lain, pemeriksaan serum untuk IgA, IgM, IgG , antibodi anti-CCP dan RF, analisis cairan sinovial, foto polos sendi, MRI, dan ultrasound (Longo, 2012).
Pengobatan dan Perawatan
RA harus ditangani dengan sempurna. Penderita harus diberi penjelasan bahwa penyakit ini tidak dapat disembuhkan (Sjamsuhidajat, 2010). Terapi RA harus dimulai sedini mungkin agar menurunkan angka perburukan penyakit. Penderita harus dirujuk dalam 3 bulan sejak muncul gejala untuk mengonfirmasi diganosis dan inisiasi terapi DMARD (Disease Modifying Anti-Rheumatic Drugs) (surjana, 2009).
Terapi RA bertujuan untuk :
a. Untuk mengurangi rasa nyeri yang dialami pasien
b. Mempertahakan status fungsionalnya
c. Mengurangi inflamasi
d. Mengendalikan keterlibatan sistemik
e. Proteksi sendi dan struktur ekstraartikular
f. Mengendalikan progresivitas penyakit
g. Menghindari komplikasi yang berhubungan dengan terapi
Terapi Farmakologik Artritis Reumatoid
Dalam jurnal “The Global Burden Of Rheumatoid Arthritis In The Year 2000”, Obat-obatan dalam terapi RA terbagi menjadi lima kelompok, yaitu (Symmons, 2006) :
1. NSAID (Non-Steroid Anti-Inflammatory Drugs) untuk mengurangi rasa nyeri dan kekakuan sendi.
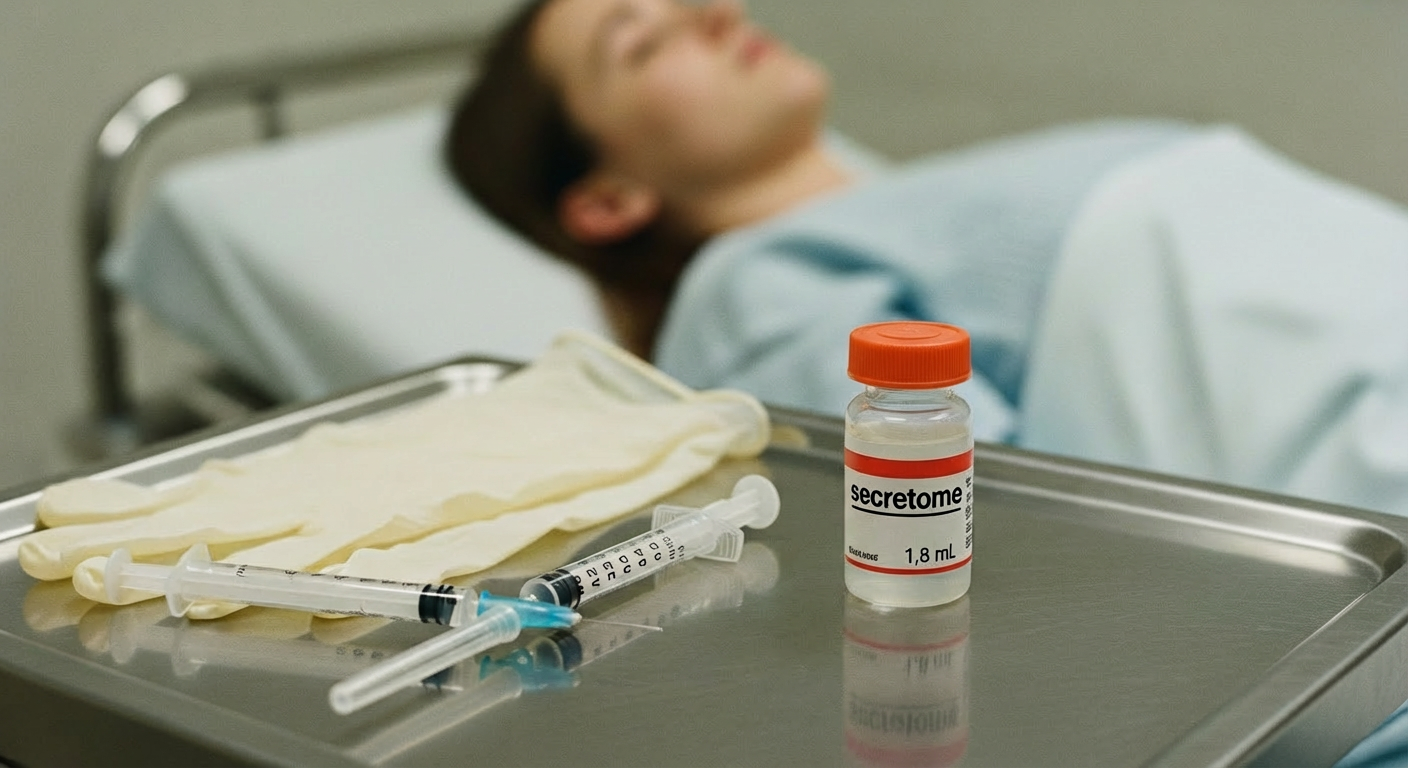
2. Second-line agent seperti injeksi emas (gold injection), Methotrexat dan Sulphasalazine. Obat-obatan ini merupakan golongan DMARD. Kelompok obat ini akan berfungsi untuk menurukan proses penyakit dan mengurangi respons fase akut. Obat-obat ini memiliki efek samping dan harus di monitor dengan hati-hati.
3. Steroid, obat ini memiliki keuntungan untuk mengurangi gejala simptomatis dan tidak memerlukan montoring, tetapi memiliki konsekuensi jangka panjang yang serius.
4. Obat-obatan immunosupressan. Obat ini dibutuhkan dalam proporsi kecil untuk pasien dengan penyakit sistemik.
5. Agen biologik baru, obat ini digunakan untuk menghambat sitokin inflamasi.
Belum ada aturan baku mengenai kelompok obat ini dalam terapi RA. DMARD (Disease Modifying Anti-Rheumatic Drugs), pemilihan jenisnya pada pasien harus mempertimbangkan kepatuhan, berat penyakit, pengalaman dokter, dan penyakit penyerta. DMARD yang paling sering digunakan adalah MTX (Metrothexate), hidroksiklorokuin atau klorokuin fosfat, sulfasalazin, leflunomide, infliximab dan etarnecept. (Suarjana, 2009).
Terapi non-Farmakologik Artritis Reumatoid
Terapi non-farmakologi melingkupi terapi modalitas dan terapi komplementer. Terapi modalitas berupa diet makanan (salah satunya dengan suplementasi minyak ikan cod), kompres panas dan dingin serta massase untuk mengurangi rasa nyeri, olahraga dan istirahat, dan penyinaran menggunakan sinar inframerah. Terapi komplementer berupa obat-obatan herbal, accupressure, dan relaxasi progressive (Afriyanti, 2009). Terapi bedah dilakukan pada keadaan kronik, bila ada nyeri berat dengan kerusakan sendi yang ekstensif, keterbatasan gerak yang bermakna, dan terjadi ruptur tendo.
Metode bedah yang digunakan berupa sinevektomi bila destruksi sendi tidak luas, bila luas dilakukan artrodesis atu artroplasti. Pemakaian alat bantu ortopedis digunakan untuk menunjang kehidupan sehari-hari (Sjamsuhidajat, 2010).
Referensi
Artritis Reumatoid. http://digilib.unila.ac.id/2424/9/2.%20Bab%202.pdf