Osteoartritis Lutut
Pendahuluan dan Fakta
Osteoartritis (OA) adalah suatu kondisi sendi yang mengalami proses degeneratif. Hal ini menyebabkan rasa sakit, bengkak, dan kaku sehingga memengaruhi kemampuan seseorang untuk bergerak bebas. Osteoartritis dapat menyerang seluruh sendi, termasuk jaringan di sekitarnya. Hal ini paling sering terjadi pada lutut, pinggul, tulang belakang, dan tangan. Osteoartritis memengaruhi sekitar 3,3% hingga 3,6% populasi secara global. Penyakit ini menyebabkan kecacatan sedang hingga berat pada 43 juta orang, menjadikannya penyakit ke-11 yang paling melemahkan di seluruh dunia.
Patofisiologi
Tulang rawan artikular atau articular cartilage terutama terdiri dari kolagen tipe II, proteoglikan, kondrosit, dan air. Tulang rawan yang sehat secara konstan akan menjaga keseimbangan antara masing-masing komponen, sehingga setiap adanya degradasi akan diimbangi dengan pembentukan tulang rawan kembali, sehingga kesehatan tulang rawan artikular tetap terjaga. Pada osteoartritis, matriks metaloprotease (MMPs), atau enzim degradatif, diekspresikan secara berlebihan, mengganggu keseimbangan dan mengakibatkan hilangnya kolagen dan proteoglikan secara keseluruhan. Pada tahap awal osteoartritis, kondrosit mensekresi penghambat jaringan MMPs dan berupaya meningkatkan sintesis proteoglikan agar sesuai dengan proses degradasi. Namun, proses reparatif ini tidaklah cukup. Hilangnya keseimbangan mengakibatkan penurunan jumlah proteoglikan meskipun terjadi peningkatan sintesis, peningkatan kadar air, pola kolagen yang tidak teratur, dan akhirnya hilangnya elastisitas tulang rawan artikular. Secara makroskopis, perubahan ini mengakibatkan retak dan pecahnya tulang rawan dan akhirnya erosi pada permukaan artikular.
Meskipun osteoartritis lutut berkorelasi erat dengan penuaan, penting untuk dicatat bahwa osteoartritis lutut bukan sekadar akibat penuaan melainkan penyakitnya sendiri. Hal ini didukung oleh perbedaan yang terlihat pada tulang rawan pada osteoartritis dan penuaan. Selain itu, enzim yang bertanggung jawab terhadap degradasi tulang rawan diekspresikan dalam jumlah yang lebih tinggi pada osteoartritis lutut, sedangkan enzim tersebut berada pada tingkat normal pada tulang rawan yang mengalami penuaan.
Etiologi
Osteoartritis lutut diklasifikasikan menjadi primer dan sekunder yang bergantung pada penyebabnya. Osteoartritis lutut primer terjadi akibat degenerasi tulang rawan artikular tanpa diketahui penyebabnya. Hal ini biasanya dianggap sebagai degenerasi yang terjadi karena usia dan keausan. Osteoartritis lutut sekunder adalah akibat dari degenerasi tulang rawan artikular karena penyebab yang diketahui.
Kemungkinan penyebab OA lutut sekunder:
- Pasca-trauma
- Pasca-bedah
- Bawaan atau malformasi anggota badan
- Malposisi (varus/valgus)
- Skoliosis
- Rakitis
- Hemokromatosis
- Chondrocalcinosis
- Okronosis
- Penyakit Wilson
- Gout
- Pseudogout
- Akromegali
- Nekrosis avaskular
- Artritis reumatoid
- Artritis psoriatis
- Hemofilia
- Penyakit Paget
- Sickle cell disease
Faktor Risiko
Dapat dimodifikasi:
- Trauma tulang artikular
- Pekerjaan
- Kelemahan pada otot atau keseimbangan
- Berat badan
- Kesehatan (sindrom metabolik)
Tidak dapat dimodifikasi:
- Jenis Kelamin
- Usia
- Keturunan
- Ras
Diagnosis
Pasien biasanya datang ke dokter dengan nyeri lutut sebagai keluhan utama. Oleh karena itu, penting untuk mengetahui riwayat gejala secara rinci. Perhatikan baik-baik riwayatnya karena nyeri lutut dapat berasal dari tulang belakang lumbal atau sendi pada pinggul. Mendapatkan riwayat medis dan pembedahan secara rinci juga penting untuk mengidentifikasi faktor risiko apa pun yang terkait dengan osteoartritis lutut sekunder.
Riwayat penyakit saat ini harus mencakup hal-hal berikut:
- Timbulnya gejala
- Lokasi nyeri tertentu
- Durasi nyeri dan gejala
- Ciri-ciri nyeri
- Faktor yang meringankan dan memberatkan
- Segala rasa sakit yang terpancar
- Waktu timbulnya gejala yang spesifik
- Tingkat keparahan gejala
- Aktivitas fungsional pasien
Gejala Klinis OA Lutut
Pada umumnya, gejala pada OA yang dialami adalah nyeri sendi atau nyeri pada lutut, yang memiliki kriteria sebagai berikut:
- Biasanya dimulai secara bertahap
- Lebih buruk lagi dengan aktivitas berkepanjangan
- Lebih buruk lagi dengan membungkuk atau tangga berulang-ulang
- Lebih buruk lagi jika tidak aktif
- Memburuk seiring berjalannya waktu
- Lebih baik dengan istirahat
- Lebih baik dengan es atau obat anti inflamasi
- Kekakuan lutut
- Lutut bengkak
- Penurunan kapasitas kemampuan jalan
Pemeriksaan fisik pada lutut dimulai dengan inspeksi visual. Saat pasien berdiri, carilah eritema (kemerahan) dan pembengkakan periartikular, atrofi (hilangnya jaringan otot) pada paha depan, dan kelainan bentuk varus atau valgus*. Amati gaya berjalan untuk mencari tanda-tanda nyeri atau gerakan abnormal pada sendi lutut yang dapat mengindikasikan ketidakstabilan ligamen. Selanjutnya, periksa kulit di sekitarnya untuk mengetahui keberadaan dan lokasi bekas luka dari prosedur bedah sebelumnya jika ada, bukti trauma, atau lesi jaringan lunak.
Pengujian rentang gerak atau range of motion (ROM) testing merupakan aspek penting dari pemeriksaan lutut. ROM aktif dan pasif berhubungan dengan fleksi dan ekstensi lutut harus dinilai dan dilakukan pendataan.
*Istilah valgus dan varus mengacu pada angulasi (atau membungkuk) di dalam batang tulang atau pada sambungan pada bidang koronal. Bila bagian distalnya lebih lateral disebut valgus. Bila bagian distal lebih medial disebut varus.
Palpasi sepanjang struktur tulang dan jaringan lunak merupakan bagian penting dari setiap pemeriksaan lutut. Pemeriksaan palpasi dapat dipecah menjadi struktur medial, garis tengah, dan lateral lutut.
Selain anamnesis dan pemeriksaan fisik yang menyeluruh, diperlukan pencitraan radiografi. Gambaran yang direkomendasikan yaitu berdiri anteroposterior (AP), berdiri menyamping dan ekstensi, dan menunjukkan gambaran patela yang terlihat jelas. Pandangan lutut posteroanterior (PA) berdiri 45 derajat dapat diperoleh, yang memberikan gambaran yang lebih baik terhadap permukaan patella yang menumpu beban.
Tata Laksana dan Perawatan
Untuk tata laksana pada OA lutut termasuk perawatan non-bedah dan pembedahan. Biasanya, penyedia layanan kesehatan mencoba perawatan non-bedah terlebih dahulu sebelum merekomendasikan dilakukannya operasi.
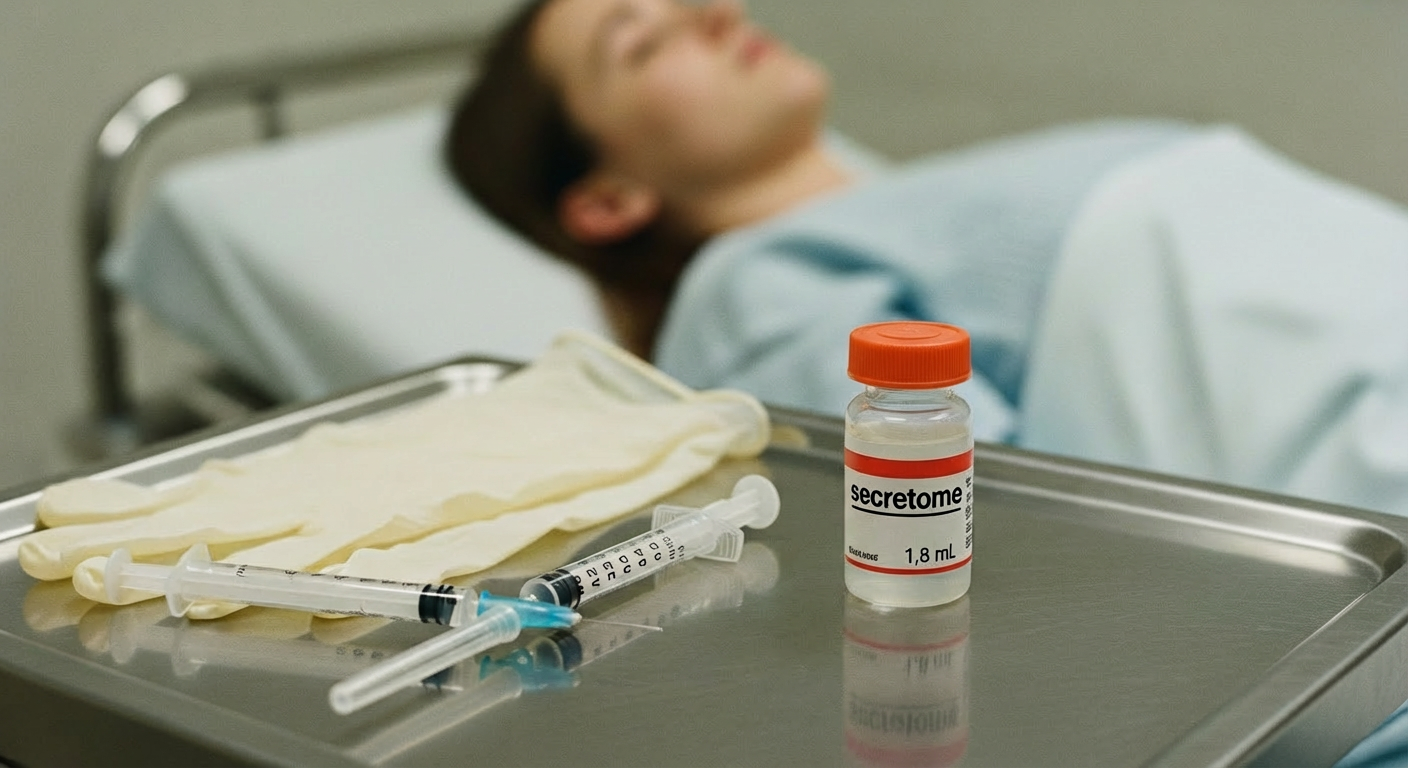
Tata laksana non-bedah:
- Menggunakan obat pereda nyeri
- Melakukan terapi fisik
- Mempertahankan berat badan yang sehat
- Menggunakan penyangga lutut
- Menggunakan orthotic seperti sol atau alas kaki khusus
- Suntikan cortisone (steroid)
Tata laksana bedah:
- Pencangkokan tulang rawan. Tulang rawan yang sehat digunakan untuk mengisi lubang di tulang rawan yang sakit
- Osteotomi lutut
- Penggantian lutut sebagian
- Penggantian lutut total
Referensi:
1. Hsu H, Siwiec RM. Knee Osteoarthritis. National Library of Medicine [Internet]. 2023. Available from: https://www.ncbi.nlm.nih.gov/books/NBK507884/
2.Cleveland Clinic. Osteoarthritis of the Knee [Internet]. 2021. Available from: https://my.clevelandclinic.org/health/diseases/21750-osteoarthritis-knee