Kehamilan Ektopik Terganggu
Pendahuluan dan Fakta
Kehamilan ektopik terganggu merupakan masalah besar di bidang ginekologi di dunia, menimbulkan morbiditas dan mortalitas maternal yang tinggi. Sejak dekade 1970-an, frekuensinya meningkat hampir 6 kali lipat di Amerika Serikat, saat ini mencapai 2% dari seluruh kehamilan. Kehamilan ektopik terganggu yang umumnya merupakan keadaan gawat darurat, bertanggung jawab terhadap 9-10% kematian maternal akibat penyakit obstetrik.
Patofisiologi
Beberapa hal dibawah ini ada hubungannya dengan terjadinya kehamilan Ektopik:
a. Pengaruh faktor mekanik. Faktor-faktor mekanis yang menyebabkan kehamilan ektopik antara lain: riwayat operasi tuba, salpingitis, perlekatan tuba akibat operasi nonginekologis seperti apendektomi, pajanan terhadap diethylstilbestrol, salpingitis isthmica nodosum (penonjolan-penonjolan kecil ke dalam lumen tuba yang menyerupai divertikula), dan alat kontrasepsi dalam rahim (AKDR). Hal-hal tersebut secara umum menyebabkan perlengketan intra- maupun ekstraluminal pada tuba, sehingga menghambat perjalanan zigot menuju kavum uteri. Faktor mekanik lain adalah pernah menderita kehamilan ektopik, pernah mengalami operasi pada saluran telur seperti rekanalisasi atau tubektomi parsial, induksi abortus berulang, tumor yang mengganggu keutuhan saluran telur.
b. Pengaruh faktor fungsional. Faktor fungsional yaitu perubahan motilitas tuba yang berhubungan dengan faktor hormonal. Dalam hal ini gerakan peristalsis tuba menjadi lamban, sehingga implantasi zigot terjadi sebelum zigot mencapai kavum uteri. Gangguan motilitas tuba dapat disebabkan oleh perobahan keseimbangan kadar estrogen dan progesteron serum. Dalam hal ini terjadi perubahan jumlah dan afinitas reseptor adrenergik yang terdapat dalam uterus dan otot polos dari saluran telur.
c. Kegagalan kontrasepsi. Alat kontrasepsi dalam rahim selama ini dianggap sebagai penyebab kehamilan ektopik. Namun ternyata hanya AKDR yang mengandung progesteron yang meningkatkan frekuensi kehamilan ektopik. AKDR tanpa progesteron tidak meningkatkan risiko kehamilan ektopik, tetapi bila terjadi kehamilan pada wanita yang menggunakan AKDR, besar kemungkinan kehamilan tersebut adalah kehamilan ektopik.
d. Peningkatan afinitas mukosa tuba. Dalam hal ini terdapat elemen endometrium ektopik yang berdaya meningkatkan implantasi pada tuba.
e. Pengaruh proses bayi tabung. Beberapa kejadian kehamilan ektopik dilaporkan terjadi pada proses kehamilan yang terjadi dengan bantuan teknik-teknik reproduksi (assisted reproduction). Kehamilan tuba dilaporkan terjadi pada GIFT (gamete intrafallopian transfer), IVF (in vitro fertilization), ovum transfer, dan induksi ovulasi. Induksi ovulasi dengan human pituitary hormone dan hCG dapat menyebabkan kehamilan ektopik bila pada waktu ovulasi terjadi peningkatan pengeluaran estrogen urin melebihi 200 mg sehari.
Gejala dan Komplikasi
Gejala dan tanda dari kehamilan ektopik:
a. Nyeri. Gejala yang muncul berkaitan dengan apakah kehamilan ektopik sudah pecah. Gejala yang paling sering dialami adalah nyeri panggul dan perut. Gejala pencernaan dan pusing atau berkunang-kunang juga sering terjadi, terutama setelah rupture. Nyeri dada pleuritik dapat terjadi akibat iritasi diafragma oleh perdarahan.
b. Haid Abnormal. Sebagian besar wanita melaporkan amenorea dengan bercak-bercak perdarahan per vagina. Perdarahan uterus yang terjadi pada kehamilan tuba sering disangka sebagai haid sejati. Perdarahan ini biasanya sedikit, berwarna cokelat tua, dan mungkin intermiten atau terus-menerus. Pada kehamilan tuba, jarang terjadi perdarahan per vagina yang hebat.
c. Nyeri Tekan Abdomen dan Panggul. Nyeri hebat pada pemeriksaan abdomen dan pemeriksaan vagina, terutama saat serviks digerakkan, dijumpai pada lebih dari tiga perempat wanita dengan rupture kehamilan tuba. Akan tetapi, nyeri tekan ini mungkin tidak ada sebelum terjadi rupture.
d. Perubahan Uterus. Pada kehamilan tuba, uterus dapat tumbuh selama 3 bulan pertama karena pengaruh hormon plasenta. Konsistensi uterus juga mungkin serupa dengan yang dijumpai pada kehamilan normal. Uterus dapat terdorong kesamping oleh massa ektopik, atau jika ligamentum latum terisi oleh darah, uterus dapat sangat terdesak. Silinder desidua uterus terbentuk pada 5 hingga 10 persen wanita dengan kehamilan ektopik. Keluarnya struktur ini mungkin disertai oleh rasa kram yang serupa dengan yang dialami saat abortus spontan.
e. Tekanan Darah dan Nadi. Sebelum pecah, tanda-tanda vital umumnya normal. Respons awal terhadap ruptur dapat berkisar dari tanpa perubahan tanda-tanda vital hingga peningkatan ringan tekanan darah, atau respons vasovagus disertai bradikardi dan hipotensi. Tekanan darah akan turun dan nadi meningkat hanya jika perdarahan berlanjut dan terjadi hipovolemia
f. Suhu. Setelah perdarahan akut, suhu mungkin normal atau bahkan rendah. Suhu dapat meningkat hingga 38°C, tetapi tanpa infeksi suhu jarang melebihi angka ini.
g. Massa Panggul. Pada pemeriksaan bimanual, dapat diraba suatu massa di panggul pada 20 persen pasien. Massa tersebut hampir selalu terletak di posterior atau lateral uterus. Massa biasanya lunak dan elastis.
h. Kuldosentesis. Kuldosentesis adalah suatu teknik sederhana untuk mengidentifikasi hemoperitoneum. Serviks ditarik ke arah simfisis dengan sebuah tenakulum, dan dimasukkan sebuah jarum panjang 16 atau 18 melalui forniks posterior ke dalam cul-de-sac. Potongan bekuan darah lama yang mengandung cairan, atau cairan mengandung darah yang tidak membeku, sesuai dengan diagnosis hemoperitoneum akibat kehamilan ektopik. Jika darah yang disedot membeku, maka darah tersebut mungkin berasal dari pembuluh darah yang tertusuk dan bukan perdarahan pada kehamilan ektopik. Tidak adanya cairan yang tersedot, tidak menyingkirkan diagnosis kehamilan ektopik
Diagnosis
Cara untuk mendiagnosa suatu kehamilan ektopik yaitu :
a. Anamesis. Pada anamneses, terdapat trias KET yaitu amenorea yang disertai tanda hamil muda, nyeri perut, bahu, tenesmus dan perdarahan pervaginam.
b. Pemeriksaan Fisik. Pada pemeriksaan dijumpai penderita tampak kesakitan, pucat, anemis, gelisah, gejala penimbunan darah dalam kavum abdomen, perdarahan dalam rongga perut dapat ditemukan tanda-tanda syok, gejala gangguan kardiovaskuler, dan gejala perubahan sistem pernafasan. Pada pemeriksaan dalam/ ginekologi terasa nyeri tekan dan nyeri goyang pada serviks, forniks posterior menonjol dan nyeri, uterus dapat teraba agak membesar, terdapat tumor dengan batas tidak jelas disekitar uterus, dan kavum douglas menonjol, berisi darah dan nyeri bila ditekan.
c. Pemeriksaan Laboratorium
1. Hemoglobin, Hematokrit, dan Hitung Leukosit. Setelah perdarahan, volume darah yang berkurang dikembalikan kearah normal oleh hemodilusi yang berlangsung dalam satu atau beberapa hari. Oleh karena itu, pemeriksaan hemoglobin atau hematokrit pada awalnya mungkin hanya memperlihatkan sedikit penurunan. Pada kehamilan ektopik terganggu, derajat leukositosis sangat bervariasi. Pada sekitar separuh wanita, dapat ditemukan leukositosis hingga 30.000/µL.
2. Pemeriksaan Urine untuk Kehamilan. Pemeriksaan urine yang tersering digunakan adalah pemeriksaan latex agglutination inhibition (hambatan penggumpalan lateks) menggunakan slidedengan sensitivitas untuk gonadotropin korion (hCG) dalam kisaran 500 hingga 800 mIU/mL. pada kehamilan ektopik, kemungkinan positif hanyalah 50 hingga 60 persen. Jika digunakan tabung, deteksi hCG adalah dalam kisaran 150 hingga 250 mIU/mL, dan uji ini positif pada 80 hingga 85 persen kehamilan ektopik. Uji yang menggunakan enyme-linked immunosorbent assay (ELISA) sensitive hingga 10 sampai 50 mIU/mL dan positif pada 95 persen kehamilan ektopik.
3. Pemeriksaan ß-hCG Serum. Radioimmunoassay, dengan sensitivitas 5 sampai 10 mIU/mL merupakan metode paling tepat untuk mendeteksi kehamilan. Karena satu kali hasil pemeriksaan serum yang positif tidak menyingkirkan kehamilan ektopik maka dirancanglah beberapa metode yang menggunakan nilai serum kuantitatif serial untuk menegakkan diagnosis. Metode ini sering digunakan bersama dengan sonografi.
4. Progesteron Serum. Satu kali pengukuran progesteron sering dapat digunakan untuk memastikan kehamilan yang berkembang normal. Nilai yang melebihi 25 ng/mL menyingkirkan kemungkinan kehamilan ektopik dengan sensitivitas 97,5 persen. Nilai yang kurang dari 5ng/mL mengisyaratkan bahwa mudigah-janin telah meninggal, tetapi tidak menunjukkan lokasinya. Kadar progesterone antara 5 dan 25 ng/mL bersifat inkonklusif.
d. Pencitraan Ultrasound
1. Sonografi Abdomen. Kehamilan di tuba falopi sulit diidentifikasi dengan sonografi abdomen. Tidak adanya kehamilan di uterus secara sonografis, uji kehamilan yang positif, adanya cairan di cul-de-sac, dan adanya massa abnormal di panggul, menunjukkan kehamilan ektopik. Sayangnya ultrasound mungkin memberi gambaran kehamilan intrauterus pada sebagian kasus kehamilan ektopik saat bekuan darah atau silinder desidua memberi gambaran seperti suatu kantong intrauterus kecil. Hal yang utama, suatu kehamilan intrauterus biasanya tidak terdeteksi dengan ultrasound abdomen hingga 5 atau 6 minggu haid atau konsentrasi ß-hCG serum lebih dari 6000 mIU / mL
2. Sonografi Vagina. Sonografi dengan transduser vagina dapat mendeteksi kehamilan uterus paling awal 1 minggu setelah terlambat haid jika kadar ß-hCG serum lebih dari 1500 mIU / mL . Uterus yang kosong dengan konsentrasi ß-hCG serum 1500 mIU / mL atau lebih sangat akurat untuk mengidentifikasi kehamilan ektopik. Identifikasi kantong gestasi dengan ukuran 1 hingga 3 mm atau lebih, yang terletak eksentrik di uterus, dan dikelilingi oleh reaksi desidua-korion mengisyaratkan kehamilan intrauterus.
3. Ultrasound Doppler Warna dan Berpulsa. Pada teknik ini dilakukan identifikasi atas letak warna vascular intra- atau ekstrauterus dalam bentuk khas yang disebut pola ring-of-fire dan pola aliran kecepatan-tinggi impendansi-rendah yang sesuai dengan perfusi plasenta. Jika pola ini terlihat di luar rongga uterus maka ditegakkan diagnosis kehamilan ektopik.
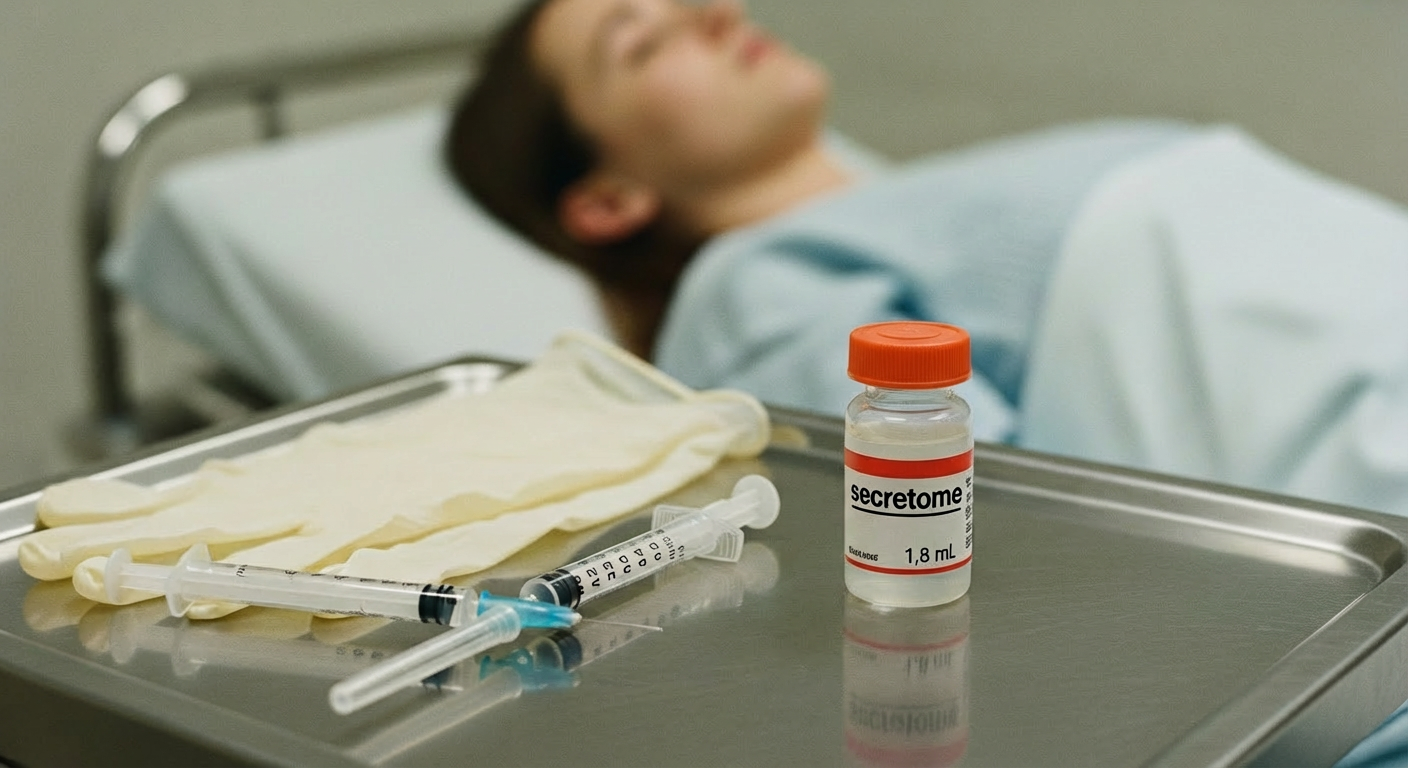
Tatalaksana dan Perawatan
Pemberian methotrexate intramuskular atau pelaksanaan operasi laparoskopi merupakan modalitas pengobatan yang aman dan efektif pada wanita yang stabil secara hemodinamik dengan kehamilan ektopik yang belum pecah. Keputusan mengenai metode mana yang akan dipilih dipandu oleh kondisi klinis pasien, temuan hasil laboratorium, dan pencitraan radiologis, serta metode pilihan pasien yang telah diinformasikan dengan baik setelah mempertimbangkan risiko dan manfaat dari setiap prosedur. Pasien dengan kadar hCG yang relatif rendah akan mendapatkan manfaat dari protokol methotrexate dosis tunggal. Pasien dengan kadar hCG lebih tinggi mungkin memerlukan regimen dua dosis. Ada literatur yang menunjukkan bahwa pengobatan dengan methotrexate tidak memiliki efek merugikan terhadap cadangan ovarium atau kesuburan. Kadar hCG harus dipantau hingga mencapai tingkat non-kehamilan setelah pemberian methotrexate.
Penanganan bedah diperlukan jika pasien menunjukkan salah satu dari berikut ini: indikasi perdarahan intraperitoneal, gejala yang menunjukkan massa ektopik yang terus berlanjut, atau ketidakstabilan hemodinamik. Manajemen bedah yang mencakup salpingostomi atau salpingektomi harus dipandu oleh status klinis, tingkat kerusakan tuba falopi, dan keinginan untuk kesuburan di masa depan. Dalam bentuk paling sederhana, salpingektomi melibatkan pengangkatan sebagian atau seluruh tuba falopi. Salpingostomi, atau salpingotomi, melibatkan pengangkatan kehamilan ektopik melalui insisi tuba dengan tetap meninggalkan tuba falopi di tempatnya.
Referensi:
- Tarigan GY. Karakteristik pasien kehamilan ektopik terganggu di RSUP H. Adam Malik periode Tahun 2012-2015. [Internet]. [Cited 26/8/2021]. Available from: http://repositori.usu.ac.id/bitstream/handle/123456789/19922/130100373.pdf?sequence=1&isAllowed=y
- Mummert T, Gnugnoli DM. Ectopic pregnancy. National Library of Medicine [Internet]. 2023. Available from: https://www.ncbi.nlm.nih.gov/books/NBK539860/