Amiotrofik Lateral Sklerosis
Pendahuluan dan Fakta
Amyotrophic lateral sclerosis (ALS) adalah penyakit neurodegeneratif yang menyerang neuron motorik. Amyotrophy menunjukkan adanya atrofi serat otot, yang diinervasi oleh anterior horn cell yang mengalami degenerasi, menyebabkan kelemahan otot dan fasikulasi. Lateral Sclerosis menunjukkan pengerasan traktus kortikospinalis lateral maupun anterior dimana neuron motorik di daerah tersebut mengalami degenerasi melalui proses gliosis (Rowland dan Shenider, 2001). Melalui gabungan istilah ini, bisa tergambarkan bahwa pada penyakit ini terjadi lesi campuran Upper Motor Neuron dengan Lower Motor Neuron.
Insidens penyakit ALS pada tahun 1990 dilaporkan antara 1,5 - 2,7 per 100.000 penduduk/tahun (rata-rata 1,89 per 100.000/tahun) di Eropa dan Amerika Utara (Worms, 2001). Insiden ALS lebih tinggi pada pria dibandingkan dengan wanita, dengan perbandingan secara keseluruhan 1,5 : 1. Menurut letak geografis, prevalensi penyakit ALS di pasifik barat termasuk daerah Guam, Pulau Mariana, Pulau Honsu dan sebelah selatan New Guinea Barat dilaporkan 50–100 kali lebih tinggi dibandingkan dengan tempat lain. Onset ALS dapat terjadi dari usia remaja hingga usia 80 tahun, namun usia insiden puncak terjadi pada usia 55-75 tahun. Onset rata- rata usia sporadis ALS (SALS) adalah 65 tahun, onset rata-rata usia familial ALS (FALS) adalah 46 tahun (Steele dan Mc. Geer, 2008).
Patofisiologi
Ciri patologis ALS adalah degenerasi dan hilangnya neuron motorik dengan gliosis astrositik dan adanya inklusi intraneuronal dalam degenerasi neuron dan glia. Patologi UMN pada ALS ditandai dengan depopulasi sel Betz di korteks motorik (area Brodmann 4), gliosis astrositik yang mempengaruhi substansia grisea dan subtansia alba sub korteks disertai hilangnya akson pada descending pyramidal motor pathway akibat gliosis dan rusaknya myelin traktus kortikospinalis (Wijesekera dan Nigel, 2009). Jumlah sel dapat berkurang hingga 50% pada otopsi pada pasien ALS.
Gejala Klinis dan Komplikasi
Penegakan diagnosis ALS berdasarkan penemuan klinis. Seseorang diduga menderita ALS jika kehilangan fungsi motorik secara bertahap atau progresif pada satu atau lebih bagian tubuh, tanpa gangguan sensoris dan tanpa penyebab jelas.
Gejala ALS biasanya belum tampak hingga penderita berusia 50 tahun, namun bisa muncul perlahan di usia muda. Gejala ALS muncul ketika neuron motorik pada otak dan medulla spinalis mulai berdegenerasi. Progresifitas ALS mungkin begitu lambat sehingga gejala awal sering diabaikan dan dianggap sebagai suatu proses penuaan (McCarthy, 2009). Bagian tubuh yang terpengaruh pada gejala- gejala awal ALS tergantung otot yang diserang pertama kali. Dalam beberapa kasus, gejala awalnya mempengaruhi salah satu kaki, dan pasien mengalami kesulitan saat sedang berjalan atau berlari dan pasien lebih sering tersandung daripada sebelumnya.
Beberapa penderita merasakan gangguan pertama kali pada tangan saat mengalami kesulitan dalam melakukan pergerakan-pergerakan sederhana yang membutuhkan keterampilan tangan, seperti mengancingkan kemeja, menulis, atau memasukkan dan memutar kunci dalam lubang kunci. Sedangkan pasien lainnya, mengalami masalah pada suara terlebih dahulu. Pada 75-80% pasien, gejala dimulai dengan keterlibatan anggota badan, sedangkan 20-25% dari pasien datang dengan gejala bulbar. Pada pasien dengan gejala bulbar, pasien dapat mengalami masalah dalam berbicara (disartria) atau penurunan volume suara. Gangguan menelan (disfagia), aspirasi atau tersedak saat makan mungkin terjadi, oleh karena terkenanya nukleus saraf kranialis VII, IX, X, XI dan XII.
Pada beberapa pasien, keluhan dapat disertai dengan perubahan kognitif. Disfungsi kognitif dialami oleh 20–50% penderita ALS, dan 3–15% berkembang menjadi demensia yang dikategorikan sebagai frontotemporal lobar degeneration (FTLD). Perubahan kognitif ditandai dengan perubahan personalitas, iritabilitas, dan defisit pada fungsi eksekutif. Diagnosis ditegakkan dengan ditemukannya gangguan kelemahan UMN dan LMN bersamaan pada anggota gerak kelemahan otot, atrofi otot, fasikulasi otot, dikombinasi dengan hiperrefleks
Diagnosis
Berdasarkan World Federation of Neurology (WFN), penegakan diagnosis dari ALS yakni:
1. Definite ALS: adanya gejala UMN dan LMN pada 3 level
2. Probable ALS: adanya gejala UMN dan LMN pada 2 level
3. Possible ALS: adanya gejala UMN dan LMN pada 1 level atau adanya gejala UMN pada 2 level
4. Suspect ALS: gejala LMN pada 2 level atau gejala UMN pada 1 level.
Dalam menggunakan kriteria WFN, ada 4 regio yang harus diketahui: Bulbar, servikal, torakal dan lumbosakral.
ALS sulit untuk didiagnosis sejak awal karena memiliki gejala mirip dengan beberapa penyakit neurologis lain sehingga diperlukan pemeriksaan tambahan untuk mengesampingkan kondisi lain. Pemeriksaan yang dapat dilakukan antara lain:
1. Elektrofisiologi
Elektrofisiologi digunakan untuk mendeteksi adanya lesi LMN pada daerah yang terlibat serta untuk menyingkirkan proses penyakit lainnya. (Wijesekera dan Nigel, 2009).
a. Konduksi saraf motorik dan sensorik. Konduksi saraf diperlukan untuk mendiagnosis dan menyingkirkan gangguan lain dari saraf perifer, neuromuscular junction, dan otot yang dapat mirip atau mengacaukan diagnosis ALS (Wijesekera dan Nigel, 2009).
b. Elektromiografi. Konsentris jarum elektromiografi (EMG) memberikan bukti disfungsi LMN yang diperlukan untuk mendukung diagnosis ALS dan harus ditemukan setidaknya dua dari empat daerah SSP: otak (bulbar), leher, toraks, atau lumbosakral medula spinalis (cornu anterior motor neuron). c. Transkranial magnetic stimulasi dan Central motor conduction studies Transkranial magnetic stimulasi (TMS) memungkinkan evaluasi non invasif jalur motorik kortikospinalis, dan memungkinkan deteksi lesi UMN pada pasien yang tidak memiliki tanda-tanda UMN.
d. Elektromiografi Kuantitatif. Motor Unit Number Estimation (MUNE) adalah teknik elektrofisiologi khusus yang dapat memberikan perkiraan kuantitatif dari jumlah akson yang mempersarafi otot atau kelompok otot.
2. Neuroimaging
Dilakukan MRI kepala/tulang belakang untuk menyingkirkan lesi struktural dan diagnosis lain pada pasien yang dicurigai ALS seperti tumor, spondilitis, siringomielia, stroke bilateral, dan multiple sclerosis (Wijesekera dan Nigel, 2009).
3. Biopsi otot dan neuropatologi
Terutama dilakukan pada pasien dengan presentasi klinis yang tidak khas, terutama dengan lesi LMN yang tidak jelas. Biopsi digunakan untuk menyingkirkan adanya miopati, seperti inclusion body myositis (Wijesekera dan Nigel, 2009).
4. Pemeriksaan lab lainnya
Tes laboratorium klinis yang mungkin abnormal dalam kasus dinyatakan khas ALS meliputi:
• Enzim Otot (serum kreatinin kinase yang tidak biasa di atas sepuluh kali batas atas normal, ALT, AST, LDH)
• Serum kreatinin (terkait dengan hilangnya massa otot rangka)
• Hipochloremia, bikarbonat meningkat (terkait dengan gangguan pernapasan lanjutan) (Wijesekera dan Nigel, 2009).
Tatalaksana dan Perawatan
Direkomendasikan riluzole (suatu antagonis glutamat) 50 mg dua kali sehari, dengan pemantauan teratur. Pemberian 100 mg riluzole oral setiap hari setelah 18 bulan memperpanjang harapan hidup penderita ALS sekitar tiga bulan. Efek samping riluzole adalah fatigue dan asthenia. Hingga kini, belum ada terapi efektif untuk ALS (Lacomblez, dkk, 1996).
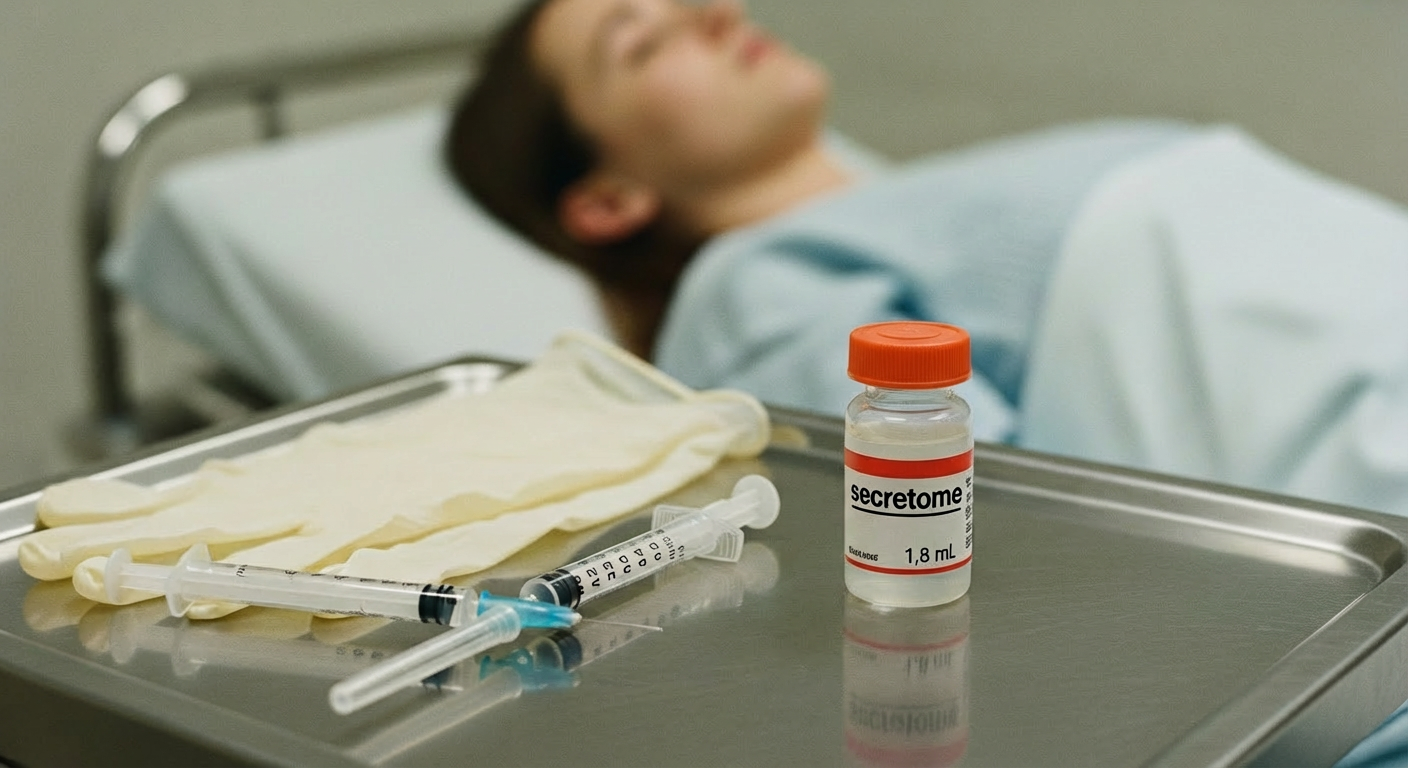
Berbagai obat sedang memasuki trial fase II/III: arimoclomol, ceftriaxone, edaravone, IGF-1 polypeptide, minocycline, sodium phenylbutyrate, tamoxifen, thalidomide. Obat yang sedang dipertimbangkan dan direncanakan memasuki trial fase III: AEOL 10150, celastrol, coenzyme Q10, copaxone, IGF-1 – viral delivery, memantine, NAALADase inhibior, nimesulide, ritonavir, hydroxyurea, scriptaid, talampanel dan trehalose (Andersen dkk, 2005). Terapi Recombinant human insulinlike growth factor (rhIGF-I) - protein manusia yang dimodifikasi secara genetik – diharapkan dapat meningkatkan dan memperkuat kelangsungan hidup neuron motorik pada ALS. Diberikan setiap hari melalui injeksi subkutan. Terapi stem cell menjanjikan, namun efektivitasnya masih memerlukan riset lanjutan
Status nutrisi penderita ALS juga perlu dievaluasi, mengingat sering terjadi disfagia, hipermetabolisme, serta beragam penyakit penyerta. Tatalaksana nutrisi termasuk diet, strategi menelan, kemungkinan dipasang selang makanan langsung ke lambung (gastrostomy tube placement), dan suplementasi berupa vitamin dan mineral (Braun dkk, 2012). Ketika status gizi terganggu oleh disfagia dan penurunan berat badan (5% -10% dari berat badan yang biasa) atau indeks massa tubuh <20 kg/m (2) tanpa kehilangan berat badan, percutaneous endoscopic gastrostomy menjadi indikasi (Greenwood,2013).
Terapi simtomatis untuk mengatasi spastisitas yang mengganggu aktivitas harian pasien adalah pemberian baclofen atau diazepam. Untuk mengatasi produksi saliva berlebihan (sialorrhea) dapat diberi trihexyphenidyl atau amitriptyline. Bila refrakter, dapat diberi injeksi botulinum toxin type B di kelenjar parotid dan submandibular. Terapi radiasi dengan dosis 7–7,5 Gy bilateral efektif mengurangi produksi saliva, namun ada efek samping, seperti: erithema dan mual (Jackson dkk, 2008).
Depresi diatasi dengan antidepresan, misalnya: amitriptyline atau golongan SSRI. Insomnia diatasi dengan amitriptyline atau golongan hipnotik, seperti: zolpidem, diphenhydramine. Cemas diatasi dengan bupropion atau diazepam 0,5 mg 2-3 kali sehari, atau lorazepam sublingual.
Afek pseudobulbar, menangis-tertawa berlebihan, atau gangguan ekspresi emosional involunter dialami 20–50% penderita ALS, terutama pada kasus pseudobulbar palsy. Kombinasi 30 mg dextromethorphan dan 30 mg quinidine dua kali sehari efektif mengatasi afek pseudobulbar. Gunakan oksigen hanya pada kasus hipoksia simtomatis.
Komplikasi pernafasan adalah penyebab umum morbiditas dan mortalitas penderita ALS. Tatalaksana insufisiensi saluran pernapasan dengan ventilasi non invasif meningkatkan kualitas dan kelangsungan hidup penderita ALS. Oksigen biasanya diberikan hanya dalam hubungannya dengan NIV untuk mencegah terhambatnya pernafasan dalam mengevaluasi kadar karbon dioksida
Referensi:
Arimbawa IK, Pramaswari AAAA. AMYOTROPHIC LATERAL SCLEROSIS (ALS). [Internet]. [Cited 29/8/2021]. Available from: https://simdos.unud.ac.id/uploads/file_penelitian_dir/a27a02ff66676c092e0a41f3948ba25e.pdf