Patients with acute coronary syndrome (ACS) undergoing percutaneous coronary intervention (PCI) usually receive dual antiplatelet therapy (DAPT), which combines aspirin with platelet receptor inhibitor P2Y12. Prasugrel and ticagrelor are usually preferred over clopidogrel among P2Y12 inhibitors, as they are better at reducing the risk of ischemic events, but with a higher risk of bleeding Determining the type and duration of DAPT most suitable for patients with ACS, however, requires a thorough examination of possible ischemic complications and bleeding.
The European Society of Cardiology in 2023 recommends a normal DAPT duration of 12 months (class I, proof level A) if the risk is relatively low. Treating patients with different risk variations requires special considerations and approaches. For example, patients with a high risk of bleeding and a low risk of thrombosis, patients with a low risk of bleeding and a high risk of thrombosis, or patients with a high risk of bleeding and thrombosis.
1. Patients with a high risk of bleeding and a low risk of thrombosis.
About 40% of patients undergoing catheterization procedures are at high risk of bleeding, for which the Academic Research Consortium has developed a useful classification system. Among these patients, those with a lower risk of recurrent ischemic events may benefit from de-escalation strategies aimed at reducing the intensity of antithrombotic therapy after standard DAPT. De-escalation may involve switching to a less potent P2Y12 inhibitor, reducing its dose, or discontinuing one of the antiplatelet agents. Trials such as TALOS-AMI and TROPICAL-ACS have shown promising results in guiding de-escalation approaches, while studies such as POPULAR Genetics and HOST-REDUCE have explored genetic and dose-based strategies. De-escalation can also involve discontinuation of one antiplatelet agent, with studies such as SMART-DATE and TICO assessing different termination approaches. Overall, European guidelines recommend considering discontinuation of DAPT in patients with high bleeding risk, with discontinuation preference after 3-6 months or 1 month, depending on individual risk assessment.
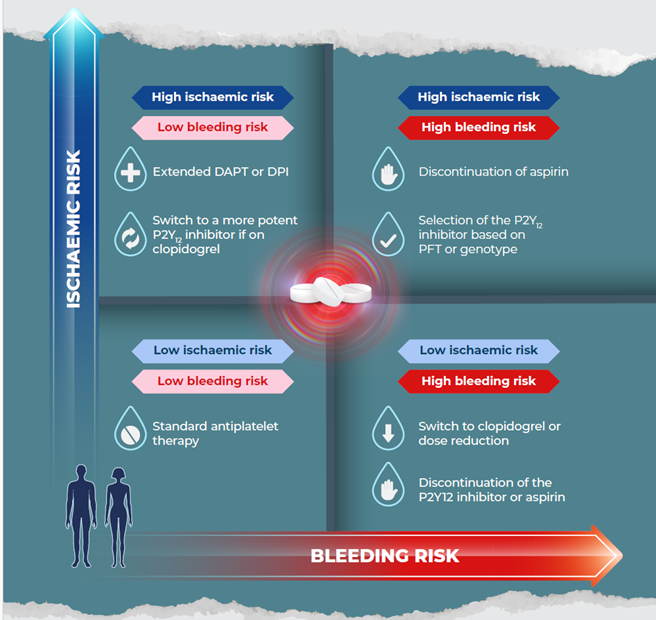
Figure 1. Personalized antithrombotic therapy strategies for patients with acute coronary syndrome undergoing percutaneous coronary intervention based on individual risk profiles. Description: DAPT, dual antiplatelet therapy; DPI, dual-pathway inhibition (i.e., the combination of aspirin and low-dose rivaroxaban); PFT, platelet function testing. (Image adapted from Capodanno D. Optimising antithrombotic therapy after ACS and PCI. 2023)
2. Patients at low risk of bleeding and at high risk of thrombosis
Identifying high ischemic risk in patients involves assessing anatomical and procedural factors, along with clinical aspects such as diabetes and multivascular disease. The Academic Research Consortium (ARC) recommends strategies such as drug enhancement for moderate to high-risk patients, with the addition of new drugs commonly used. Studies such as PEGASUS-TIMI 54 and COMPASS show the efficacy of adding low-dose ticagrelor or rivaroxaban to aspirin in reducing ischemic events. European Society of Cardiology guidelines recommend considering the addition of low-dose P2Y12 or rivaroxaban receptor inhibitors for patients at high ischemic risk and low risk of bleeding. For moderate ischemic risk and low bleeding risk, this recommendation is slightly lower. In summary, patients with high ischemic risk and low bleeding risk may benefit from additional treatment, while drug switching may also be considered if needed.
3. Patients at high risk of bleeding and at high risk of thrombosis
In patients with a high risk of ischemic and bleeding, the MASTER-DAPT study found that reducing the risk of bleeding did not increase ischemic events. However, direct comparisons between various strategies such as dose discontinuation, switch, or reduction are minimal. An indirect analysis showed that discontinuation of the dose reduced bleeding, while switching or reducing the dose reduced ischemic events and hemorrhage. The amount of medication used certainly affects bleeding risk, but testing platelet function and genotype is not routinely recommended. However, individual treatment decisions, taking into account patient preferences and clinical profile, are crucial. Thus, for patients with a high risk of ischemic and bleeding, strategies such as aspirin discontinuation or selection of P2Y12 receptor blockers based on platelet or genotype testing can be considered, with collaboration between the patient and the healthcare team essential.
Conclusion
Dual Anti-Platelet Therapy plays an important role in the management of ACS patients. Various strategies and recommendations have been provided to ensure the best end result for ACS patients. Ultimately, individualized treatment decisions should be made through collaboration with the patient's healthcare team, taking into account the available evidence as well as the patient's specific clinical profile, values, and preferences.
Abbreviation: ACS: Acute Coronary Syndrome; DAPT: dual antiplatelet therapy; PCI: Percutaneous Coronary Intervention; ARC: Academy Research Consortium, PFT: Platelet Function Testing
Picture downloaded from <a href="https://www.freepik.com/free-photo/asian-doctor-visit-examines-senior-man-home-doctor-checking-up-consulting-retirement-health-partienthospital-services-wearing-mask-protect-covid19_25830808.htm#page=3&query=heart%20doctor%20patient&position=9&from_view=search&track=ais&uuid=5ce0c9d0-13a9-413e-ab4d-9f59f7487635">Image by partystock</a> on Freepik)
Reference:
Capodanno D. Optimising antithrombotic therapy after ACS and PCI. Vascul Pharmacol. 2023 Dec; 153:107228. doi: 10.1016/j.vph.2023.107228. Epub 2023 Sep 17. PMID: 37717709
ID-PLA-2024-01-IESJ (01/24)