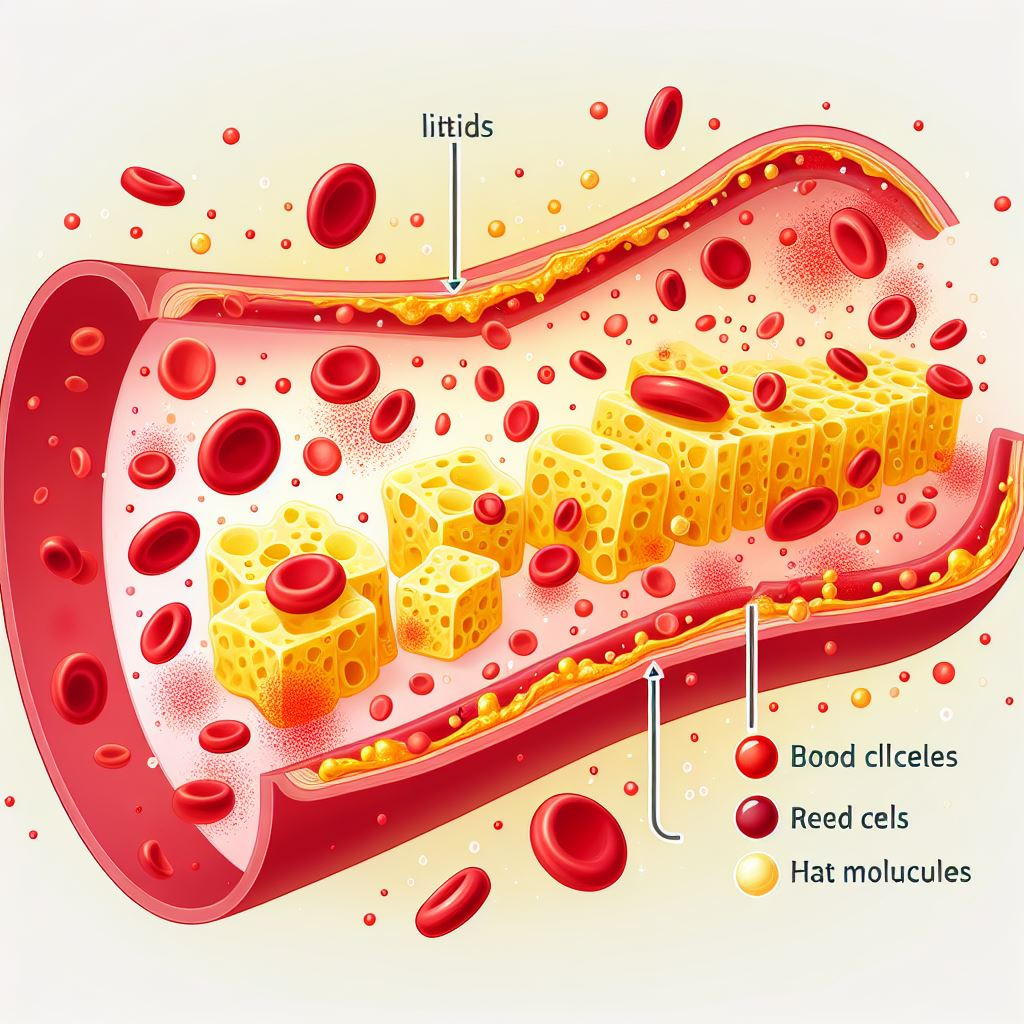
Amlodipine is a long-acting calcium channel blocker (CCB) antihypertensive with relatively minimal side effects related to its vasodilating effect. Hence, amlodipine is commonly used for hypertension therapy, but has not been used in pregnant women. Studies have reported that as a class, CCBs do not cause significant teratogenic effects (abnormal development of cells during pregnancy leading to damage to the embryo), even if given early in pregnancy.
Since information on specific CCBs is limited, a study was conducted to evaluate the safety of amlodipine in pregnancy, especially when administered in the first trimester, compared to pregnant women with chronic hypertension who received non-amlodipine antihypertensives or who did not use antihypertensive drugs.
This retrospective study analyzed medical record data over an 8-year period from pregnant women with chronic hypertension who delivered live babies. Chronic hypertension was defined as hypertension diagnosed before pregnancy or before 20 weeks gestation. Pre-eclampsia, gestational hypertension, postpartum hypertension, white-collar hypertension, and pulmonary hypertension were excluded from the study. Hypertension was defined as systolic blood pressure ≥140 mmHg or diastolic blood pressure ≥90 mmHg at 2 measurements.
Based on maternal medical record data of live-born infants, exposure of pregnant women to antihypertensive drugs during the first trimester (the time period from conception to 11 weeks 6 days gestation) was assessed. Pregnant women and their fetuses exposed to amlodipine in the first trimester were categorized as group A, while those exposed to other antihypertensives were categorized as group O. Meanwhile, those not exposed to antihypertensives were categorized as group N. The primary outcome evaluated in this study was the incidence of major congenital anomalies in the three therapy groups.
As a result, from the medical record data, a total of 1,624 infants born to pregnant women with hypertension were obtained, of which 231 pregnant women met the criteria for analysis. Of the 231 subjects, 48 subjects were categorized in group A, 54 subjects in group O, and 129 subjects in group N. There were no differences in the baseline characteristics of the subjects between groups, except that in Group A there were more women with thyroid disorders, a history of hypertension in previous pregnancies, and stunted fetal growth. Group O had a greater gestational age at delivery than Group N.
Congenital anomalies were observed in 11 out of 231 infants: 2 of 48 in group A (4.2%), 3 of 54 in group O (5.6%), and 6 of 129 in group N (4.7%). There was no difference in the incidence of congenital anomalies between the three groups. There was no difference in labor output between all groups. The type of congenital malformation reported with amlodipine was cardiac malformation, while the congenital malformations reported with other antihypertensives were cardiac malformation and hypospadias. The types of abnormalities found were included in the types of abnormalities reported in the group that did not receive antihypertensives. Maternal hypertension has been shown to be associated with cardiac malformations, hypospadias, and esophageal atresia/stenosis in previous studies. In this study, there was no increased risk of morphologic abnormalities in the antihypertensive-exposed versus non-exposed group (Group A+O vs. N; p=0.929).
Conclusion:
The incidence of congenital anomalies in infants born to first trimester pregnant women exposed to amlodipine is not significantly different from those exposed or not exposed to other antihypertensives.
Image: Illustration (Source: pexels)
Reference:
Mito A, Murashima A, Wada Y, Miyasato-Isoda M, Kamiya CA, Waguro M, et al. Safety of amlodipine in early pregnancy. J Am Heart Assoc. 2019; 8:e012093.