Nail psoriasis is found in up to 80% of patients with skin psoriasis. Nail psoriasis is considered a condition that causes significant physical and emotional burden, thereby impacting patients' quality of life. Research has found that BoNT-A injections show promise as an alternative therapy.
The pathogenesis of nail psoriasis is still not fully understood. Several studies have shown an increase in nerve fiber concentration and neuropeptide levels, including calcitonin gene-related peptide and substance P, in psoriatic skin. The expression of these neuropeptides may contribute to the occurrence of acanthosis and immune cell infiltration in psoriatic skin. The use of botulinum toxin A (BoNT-A) has shown promising results, both in animal models and in clinical trials of skin psoriasis. BoNT-A has been shown to be effective in improving acanthosis and reducing neuromodulators in mouse models with psoriasis-like dermatitis.
Several studies have reported the effectiveness of BoNT-A in resistant plaque psoriasis or inverse psoriasis. Recently, two cases of successful nail psoriasis therapy after a single BoNT-A injection were reported. This study aims to assess the potential of intralesional BoNT-A injection as a new therapeutic approach for nail psoriasis. This study is a prospective, randomized, intraindividual control trial. Nail psoriasis was diagnosed clinically. Each participant had at least 4 fingernails with psoriasis, with a Nail Psoriasis Severity Index (NAPSI) score of at least 3 points per nail. Individuals with a history of allergy to botulinum toxin products, vitamin D, corticosteroids, cow's milk protein, or lidocaine were excluded from the study.
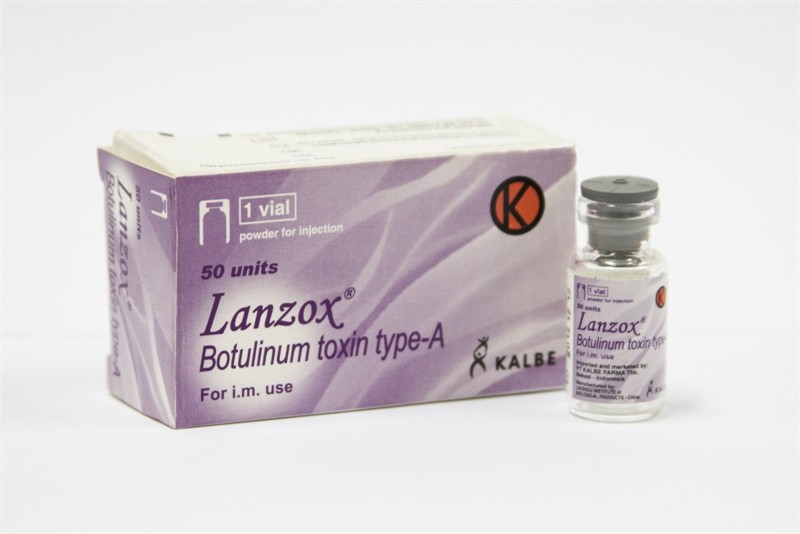
Each patient underwent four different therapeutic modalities, namely BoNT-A, triamcinolone acetonide (TA), topical vitamin D and steroids, and placebo. These four therapeutic groups were randomly assigned to each psoriatic nail using a computer program. In the BoNT-A group, psoriatic nails were injected intralesionally with 0.05 mL of BoNT-A per site (7.5 U per site) at week 0. The TA group received intralesional injections of TA (10 mg/mL) at 0.05 mL per site on psoriatic nails at week 0 and week 8. Participants in the vitamin D and steroid group used calcipotriol/betamethasone dipropionate topical ointment once daily on psoriatic nails for 16 weeks. Meanwhile, in the placebo group, nails received no therapy for 24 weeks. Intralesional injections were performed using a modified De Berker technique. The number of injection sites varied according to the location of psoriatic lesions.
The evaluator assessed the Nail Psoriasis Severity Index (NAPSI) score on 4 fingernails, measured at the start of the study (week 0), week 8, week 16, and week 24 using a dermatoscope. Each nail was visually divided into 4 quadrants with imaginary horizontal and longitudinal lines. Each quadrant was scored for nail matrix psoriasis, including pitting, leukonychia, red spots on the lunula, and nail plate damage (0–4), as well as nail bed psoriasis, including onycholysis, flaky bleeding, oil drop color changes, and nail bed hyperkeratosis (0–4). The total sum of these scores provides an overall NAPSI score for each nail (0–16). During each injection procedure, participants were asked to rate their pain level on a scale of 0 to 10 (0 = no pain, 10 = most severe pain).
Results:
· This study involved 16 patients with a total of 64 psoriatic nails who successfully completed follow-up for 24 weeks.
· The average age of the patients was 45 years (range 30–71 years). More than half of the participants were male. All participants had plaque psoriasis, with an average Psoriasis Area and Severity Index (PASI) score of 4.7 and an average disease duration of 11 years. The average body mass index was in the overweight category.
· At baseline, the average NAPSI target score was approximately 7.7. There were no significant differences between the treatment groups. At week 16, all three regimens showed significant improvement in nail condition compared to baseline (p < 0.01). After a single BoNT-A injection, the total NAPSI target decreased gradually by almost 40% (p = 0.008). With TA injections every 8 weeks, the total NAPSI target decreased by 50% (p = 0.001), while the combination of topical vitamin D and steroid therapy showed a change of approximately 30% (p = 0.003). Interestingly, at the 24-week follow-up, the BoNT-A group continued to show a positive trend of nail improvement, while the TA group tended to stabilize. However, no significant differences were found between the BoNT-A and TA groups at any time point.
· At weeks 16 and 24, all three therapeutic approaches resulted in a significant reduction in the baseline NAPSI nail score (p < 0.05). At week 16, BoNT-A injections (p = 0.02) and TA (p = 0.01) showed a reduction of approximately 40% in the baseline NAPSI nail score. Interestingly, at week 24 there was a significant difference in nail bed changes between all therapies (p = 0.002). Nail bed improvement could reach up to 60% after a single BoNT-A injection (p = 0.003), while results with TA injections remained stable since week 16. The difference in changes during this follow-up period was significant between the BoNT-A and TA regimens (p = 0.038).
· No serious side effects from either injections or topical therapy were reported throughout the study.
Conclusion:
Nail psoriasis affects up to 80% of patients with skin psoriasis and has a significant impact on quality of life, but existing therapies remain limited. This study demonstrates that BoNT-A injection shows promise as a new alternative therapy for nail psoriasis with sustained improvement despite only a single injection.
Figure: Illustration (Source: Gustavo Fring-Pexels)
Reference:
Juntongjin P, Srisinlapakig S, Nitayavardhana S. Botulinum toxin injection shows promise in nail psoriasis: A comparative randomized controlled trial. JAAD Int. 2024 Sept 1;16:105–11.